You wake up one morning, your upper gums feel oddly stiff, puffy and tender. Alongside that, you’ve got a stuffy nose, a bit of pressure around your cheeks and temple, maybe a mild headache. Your mind races: is this a gum infection? A dental issue? Or could the culprit be somewhere seemingly unrelated, like your sinuses?
That leads to the central question: can a sinus infection cause swollen gums? And if so, what does that mean for your oral health, what can you do about it, and when should you see a doctor or dentist? Let’s find out more if sinus is the reason for your swollen gums.
Getting Oriented: Sinus And Gum Swelling
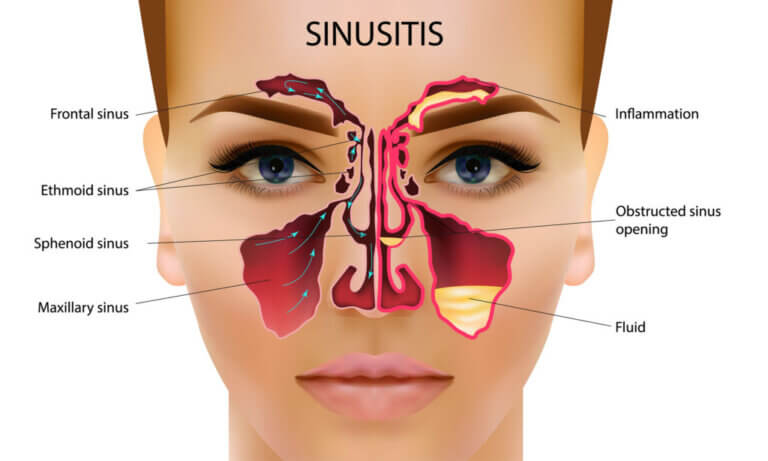
Sinus Basics
Your sinuses are air-filled cavities around your nose and cheeks and behind your forehead. When they become inflamed, called sinusitis, you get congestion, pressure, thick mucus, headaches, and sometimes pain in the upper teeth. Because the roots of your upper teeth and your maxillary sinus sit so close together, inflammation can indirectly show up in your mouth. That’s why we always wonder: can a sinus infection cause swollen gums?
Gum Inflammation And Gum Disease
Gums (gingiva) are soft tissues which hold in place your teeth and also cover the underlying bone. When they are annoyed, either as a result of plaque, infection, or some other cause, you experience gum inflammation. It can manifest as redness, swelling, tenderness and even bleeding. When left unchecked, this progresses to gingivitis or even periodontitis. So when your gums swell, you’re right to take notice.
Quick Link Between the Two
Since the maxillary sinus sits just above the roots of the upper molars and premolars, any inflammation in that area can potentially put pressure on those roots or the alveolar bone. This may result in referred pain, gum soreness and certain forms of swelling. Yes, does swollen gums come as a result of a sinus infection? Briefly: yes, but in some circumstances we will see how and why.
How a Sinus Issue Might Lead to Gum Symptoms?

Think of it in this way: the sinus is one compartment, your gums are another, and there’s a little “shared wall” between them. If the sinus inflames, the pressure, fluid or infection might “leak” metaphorically into the gum area.
Here are some key ways that happens:
-
Bone and root adjacency: The roots of some upper teeth especially are very near the floor of the maxillary sinus. When sinus pressure builds, that root-sinus “ceiling” gets stressed, and you can feel an ache or your gums might puff slightly.
-
Referred pain: Your body sometimes “mis-reads” the source of pain. Gum pain might actually be sinus in origin, or vice versa.
-
Infection spread: Rarely, an untreated sinus infection can lead to bone (osteitis) or tooth root inflammation (apical periodontitis) which affects the gums.
-
Inflammatory mediators: When your sinus is inflamed, your immune system is active; the same inflammatory chemicals might spill over into adjacent tissues including gum tissue, causing swelling.
So yes, can a sinus infection cause swollen gums? Mechanically, yes: it doesn’t always happen, but the anatomical and physiological links are there.
Common Symptoms: When You Suspect Both Sinus And Gum Issues
|
Symptom |
Likely Sinus-Origin |
Likely Gum-Origin |
|
Facial / cheek pressure |
Often present (maxillary sinus) |
Rare (except if gum-abscess) |
|
Upper tooth/gum discomfort |
Possible (especially upper molars) |
Common (gum disease, gingivitis) |
|
Gums appear red/swollen/bleeding |
Less common unless secondary issue |
Very likely |
|
Nasal congestion / runny nose |
Yes |
Generally no |
|
Bad taste or bad breath |
Less likely |
Yes — if gum disease present |
|
Tooth sensitivity to hot/cold |
Sometimes (via sinus pressure) |
Often (gum recession, root exposure) |
|
Purulent (pus) discharge |
Possible if sinus infection |
Possible if gum abscess |
This helps you see that there is overlap, which is why it becomes tricky. So when you’re asking yourself can a sinus infection cause swollen gums, you’re actually dealing with a mix of shared symptoms, which means you need to dig a little deeper.
Risk Factors That Make You Prone to This Double Trouble
Here’s a bullet-point list (for change of pace) of things that raise the odds of “sinus + gum symptoms”.
-
Chronic or recurrent sinus infections / sinusitis.
-
Allergies, nasal polyps or structural nasal problems (lead to sinus pressure).
-
Upper molar/premolar roots particularly close to the sinus floor (some people more than others).
-
Poor oral hygiene (dental plaque, periodontal disease).
-
Smoking, diabetes, immune compromise (these worsen gum disease).
-
Post-nasal drip in sinusitis causing acidic/mucous environment in mouth.
-
Dry mouth (xerostomia) happens with some sinus medicines and reduces the mouth's natural protective saliva, increasing gum inflammation risk.
If you check several of these, you’re in the “higher risk” category where a sinus infection causing swollen gums becomes a worry worth addressing.
Why Your Dentist Might Miss the Sinus Link And What to Ask?
Misdiagnosis Happens
Because dentists focus on teeth and gums, they may see swollen gums and jump to gum disease, without considering the sinus link. Meanwhile, doctors treating sinus issues may not look inside your mouth, so the root cause is missed.
What to Ask Your Healthcare Provider
-
“Could the upper gum swelling I’m showing you be related to my sinus/ nasal symptoms?”
-
“Would a sinus radiograph or CT scan help determine if there’s a sinus-tooth/gum link?”
-
“Can we check for gum disease (gingivitis/periodontitis) along with treating my sinus inflammation?”
-
“Are there medications or strategies to reduce sinus pressure that might ease my gum swelling?”
Integrated Approach Wins
If you and your healthcare/dental team ask the right questions, you cover both bases. This is exactly the scenario where asking can a sinus infection cause swollen gums becomes more than just academic; it becomes very practical.
Treatment Strategies: Re-Line the Coping Plan

Let’s walk through what you can do, step by step. Mix of explanation + actionable steps.
Step 1: Address the Sinus Component
-
It is the case with nasal congestion, facial pressure, thick mucus: visit an ENT or primary care.
-
Over-the-counter decongestants, saline nasal rinse, and steam inhalation can help relieve sinus pressure.
-
If bacterial sinusitis is suspected: antibiotics (only when indicated).
-
Sinus-irrigation (neti pot, saline spray) helps reduce inflammation.
-
Manage underlying triggers like allergies or nasal structural issues.
Step 2: Focus on Gum Health
-
Brush twice daily with a soft-bristle brush; floss daily, core of managing gum inflammation.
-
Use an antimicrobial mouth rinse if your dentist recommends it.
-
When your gums bleed, your teeth hurt, or your gums have receded: you may have gum disease.
-
The Goodbye Company Gum Disease oral solution will come in at this point. And in case you have bad oral health like bleeding gums, tooth ache or being sensitive to hot or cold temperatures - incorporate this all natural solution into your daily routine.
Wildly enriched with Omega 3 and 9 oils, neem and clove essential oils, it prevents and treats gingivitis and helps in healing the natural gums. Use it as your natural solution to gum disease and as an addition to your oral-care kit.
Step 3: Combine and Monitor
-
After starting both sinus treatment and improved gum hygiene, monitor your progress.
-
If gum swelling persists despite sinus relief, then the likely cause is gum-originated (periodontal disease) rather than sinus.
-
If sinus symptoms improve but you still feel upper jaw/teeth discomfort plus gum puffiness, revisit your dentist for root/jaw evaluation (apical periodontitis or root-sinus contact).
-
Don’t ignore ongoing issues: sustained gum swelling might lead to deeper bone loss, infection or systemic health issues.
Seasonal Triggers: Why Sinus-Induced Gum Swelling Is Worse in Certain Months

If your gums randomly start swelling every spring or winter, you’re not imagining it, your sinuses are seasonal drama queens, and your gums are innocent bystanders. Certain times of year create the perfect storm for sinus pressure, mouth breathing, and inflammation, which all team up to make your gums feel puffy, sore, and angry.
Spring and Fall Allergy:
Let’s start with spring and fall allergy seasons. When pollen levels spike, your sinuses go into defensive mode, cue congestion, inflammation, and postnasal drip. That sinus pressure sits right above your upper gums, so the more swollen your sinuses are, the more pressure and pain your gums feel.
Add in mouth breathing (thanks, stuffed nose), and your gums dry out faster, making them more sensitive and inflamed.
Winter Allergy:
Then comes winter, the dry air villain. Cold weather outside and indoor heating inside means low humidity everywhere. Dry air sucks moisture from your nasal passages and your gums. When your mucous membranes dry out, they lose their protective barrier, which can lead to irritation, soreness, and even bleeding. Plus, winter colds and sinus infections increase mucus buildup and pressure in..you guessed it; the sinus areas connected to your gums.
And don’t forget medications. Allergy pills, decongestants, and cold remedies often cause dry mouth, which reduces saliva. Saliva keeps bacteria under control, so when your mouth is dry, bacteria multiply and your gums become inflamed much faster.
Thankfully, you can prepare seasonally:
-
Use a humidifier in winter.
-
Start allergy meds or nasal rinses before allergy season hits.
-
Stay hydrated year-round.
-
Keep up with dental hygiene, even when you’re sick.
-
Consider switching to sinus-safe or mouth-friendly medication alternatives.
Bottom line: Your gums might be telling you more about the WEATHER than your brushing habits.
Home Remedies vs Medical Treatment: Which is Viable?
When your gums are swollen from sinus pressure, the first thought isn’t “Let me schedule an appointment.” It’s “What do I have at home that can fix this right now?” But not all remedies work, and some “natural hacks” floating around the internet are… questionable. Here’s what actually helps,and when it’s time to call in backup.
Home Remedies That Actually Work
Saltwater Rinse: Classic for a reason. It reduces bacteria, soothes inflammation, and promotes healing. Gentle, cheap, and dentist-approved.
Steam Inhalation or Hot Shower: Softens mucus, opens sinus passages, and reduces the pressure sitting on your gums.
Warm Compress on Sinuses: Relieves congestion and improves circulation, easing gum pain caused by sinus pressure.
Ice on the Gums: Good for immediate swelling relief. (Just don’t overdo it, 10 minutes at a time.)
Home Remedies That Are Overhyped or Risky:
-
Straight essential oils on gums (too harsh).
-
Alcohol-based mouthwash (dries the tissue more).
-
“Just push the mucus out” hacks (please no).
Medical Treatments That Help
-
Nasal Sprays (saline or steroid): Reduce sinus inflammation directly.
-
Decongestants: Great for short-term relief, but can dry out your mouth.
-
Antibiotics: Only if a bacterial infection is confirmed.
-
Dental Cleaning or Checkup: If bacteria build-up is contributing to the swelling.
When Is Home Care Enough?
-
Mild swelling.
-
Only during colds/allergies.
-
Improves with rinses, steam, and hydration.
When to See a Doctor or Dentist?
-
Gum swelling lasts more than a week.
-
Pain becomes severe or throbbing.
-
You notice pus, bad smell, or fever.
-
One specific gum area swells repeatedly.
-
You’re unsure if it’s sinus or periodontal (let a pro decide).
Bottom line: Use home remedies for comfort and symptom control, but don’t ignore persistent swelling. Sometimes your body isn’t asking for coconut oil… it’s asking for a doctor.
When to Worry (Red Flags)

If you’re wondering can a sinus infection cause swollen gums, here are the ‘uh-oh’ signs you shouldn’t ignore:
-
Severe tooth pain, hot/cold sensitivity, pus around a gum line.. may indicate a dental abscess rather than just sinus spillover.
-
High fever, facial swelling, worsening headache, especially after a sinus issue, could signal a serious sinus infection or spread to bone.
-
Gums receding rapidly, loose teeth, deep pockets: These are clear signs of advanced gum disease (periodontitis), needing prompt dental care.
-
Persistent sinusitis + gum symptoms for more than 2-3 weeks - if you’ve been treating and no improvement, time to get evaluated.
-
Vision changes, swelling around the eyes, severe facial pain. Quite rare but possible complications of sinus infections, requires emergency care.
In these cases, don’t wait. Whether the origin is sinus or dental, you need prompt attention.
Myth-Busting & Common Misconceptions
Myth #1: “Swollen gums always mean gum disease”
Not true. While gum disease is a major cause of gum swelling, sometimes the root cause is adjacent inflammation - such as from a sinus issue. So if you’re thinking “can a sinus infection cause swollen gums”, yes, that’s exactly part of busting this myth.
Myth #2: “Sinus pain can’t affect the mouth”
False again. Because of anatomical proximity, sinus issues can manifest as dental/gum symptoms. Many people mis‐attribute tooth pain to cavities when it’s really sinus pressure.
Myth #3: “If I treat my gums, the sinus symptoms will go away”
Not necessarily. If your sinus is the primary issue, brushing and flossing alone won’t fully resolve that pressure. You’ll need to treat the sinus inflammation too. A dual approach is often required.
Myth #4: “Natural solutions don’t work for gum or sinus problems”
Actually, many people find relief with non‐invasive, natural options. For example, the product - The Goodbye Company Gum Disease oral solution, uses Omega 3 & 9 oils, neem, and clove to support gum health naturally. While it’s not a substitute for medical advice when needed, it’s a solid preventive/maintenance strategy.
Prevention And Lifestyle Habits
Good Daily Habits
-
Brush & floss consistently - primary defense against gum inflammation.
-
Use a natural oral-care product - as an adjunct to your normal routine.
-
Keep your sinuses clear - saline rinses, steam, keep allergies under control.
-
Stay hydrated - helps thin mucus and supports oral health.
-
Avoid tobacco - smoking increases both sinus issues and gum disease risk.
-
Eating anti-inflammatory foods - fatty fish (Omega-3 source), leafy greens, nuts help reduce systemic inflammation.
-
Manage allergies - persistent nasal congestion can perpetuate sinus pressure, which may then affect your gums.
-
Visit your dentist and ENT regularly - especially if you have recurring symptoms.
-
Recognize signs early - if you notice gum swelling + sinus pressure, ask: can a sinus infection cause swollen gums? It’s a good check-in to your body.
Lifestyle Tweaks for Bonus Support
-
Sleep with your head elevated to reduce sinus drainage at night.
-
Use a humidifier if your nose/mouth gets dry (dry air can irritate gums and sinuses).
-
After nasal rinse or decongestant, rinse mouth to remove any residual salts/irritants that might affect gum tissue.
-
Be cautious with certain mouthwashes (high alcohol) if your gums are already sensitive; they can dry the tissues and worsen inflammation.
When the Product Fits Into Your Daily Life
If right now you’re dealing with any of the following: bleeding gums, tender swollen gums, tooth pain, sensitivity to hot/cold, it’s time to add something strong to your toolkit. That’s where Gum Disease oral solution comes in. Let us tell you how it works and why it fits perfectly when you’re concerned with questions like can a sinus infection cause swollen gums.
What it contains
-
Omega 3 & 9 oils: These fatty acids support anti-inflammatory responses in your gums, helping the tissue calm down and recover.
-
Neem (Azadirachta indica): A natural plant extract with antimicrobial, anti-inflammatory and antiseptic properties.
-
Clove essential oil: Long used in dentistry for its soothing and numbing effect; helps reduce gum soreness and sensitivity.
-
It’s all-natural, so for many people who prefer non-chemical options, it’s a really good fit.
How to use it
-
Use after brushing and flossing, as part of your nighttime routine (and optionally morning if your gums are really sensitive).
-
Swish for the recommended duration (as per label) so the active oils reach the gum-tooth junction.
-
If you’ve had a recent sinus episode that’s also impacted your upper gums, this product gives your gum tissue extra support while you work on the sinus side (nasal rinse, decongestants, ENT follow-up).
Why it’s especially relevant
If you’re asking “can a sinus infection cause swollen gums”, then you’re already thinking “there may be an extra layer here besides just my oral hygiene.” That’s exactly when you want a dual approach: treat the sinus side AND bolster the gum side. The Goodbye Company product helps prevent and treat gingivitis, which means it’s not just masking symptoms - it’s supporting healthy gum tissue long-term.
Final friendly note
Of course, if you have severe symptoms, gum abscesses, or suspected bone involvement, you should absolutely see your dentist or doctor. But for many of us managing mild-to-moderate gum inflammation, adding a strong natural solution like this into your daily routine is a smart, proactive move.
FAQs - Can A Sinus Infection Cause Swollen Gums
How do you know if it’s sinus pain or a dental issue?
The symptoms can overlap, but there are clues.
-
Sinus pain tends to worsen when you lean forward, and often comes with nasal congestion or thick mucus.
-
Dental pain/gum swelling tends to be more localized around a specific tooth or gum area, might respond to warm salt-water rinse, and is often worse when you bite down or press the gum.
-
If your gums are visibly swollen or bleeding, and you don’t have nasal congestion, likely a dental/gum issue.
-
If you have nasal symptoms + upper jaw discomfort + your dentist says “teeth look fine”, consider sinus origin.
Can untreated sinusitis lead to gum disease?
While it’s not the most common cause of gum disease, an untreated chronic sinus infection can contribute to an inflammatory burden that worsens existing gum problems. So yes.. indirectly, it can make gum disease worse or harder to manage.
Will gum swelling always go away once the sinus is treated?
Not always. If there is underlying gum disease, you’ll need specific gum treatment (cleaning, improved hygiene). Treating just the sinus may reduce pressure but won’t fix gum-organised problems entirely.
Can I use just a water nasal rinse and skip the dentist if I suspect this link?
You can, but it’s risky. Because if your gums are swollen due to gum disease not sinus, then delaying dental care allows progression. So check both.
How long after sinus relief should gum swelling go down?
If the gum swelling is indeed due to sinus pressure, you might see improvement within a week of sinus relief + good oral hygiene. If there is no improvement in 2–3 weeks, follow up with a dentist.
Is The Goodbye Company Gum Disease oral solution safe with other oral products?
Yes, it’s designed to complement brushing/flossing. Just ensure you follow the usage instructions and inform your dentist if you have any allergies.
Outlook
So, we’ve covered a lot. We asked: can a sinus infection cause swollen gums? The answer is yes, it can. But it’s not always the reason. Sometimes it’s strictly a gum problem; other times it’s a sinus issue masquerading as a gum problem; and often it’s a little of both.
Here are your take-home bullet points:
-
Don’t assume swollen gums automatically mean classic gum disease. Consider the sinus connection.
-
If you have upper-jaw gum swelling + nasal congestion/facial pressure = suspect the sinus link.
-
Treating both sides: sinus hygiene (nasal rinses, decongestants, allergy care) + oral hygiene (brushing, flossing, supportive products like The Goodbye Company Gum Disease) is the gold-standard approach.
-
If symptoms persist, escalate: dentist + ENT collaboration is key.
-
Stay consistent with your self-care: natural oral solution, avoid tobacco, eat anti-inflammatory foods, manage allergies; all help reduce that underlying inflammatory load.
And finally, if you’re ever in doubt whether your gum issue is “just gums” or something more complex like sinus-related, ask yourself: can a sinus infection cause swollen gums? If the answer is “maybe”, then you’re already half-way to the solution.