What Is A Spider Vein Or Telangiectasia?
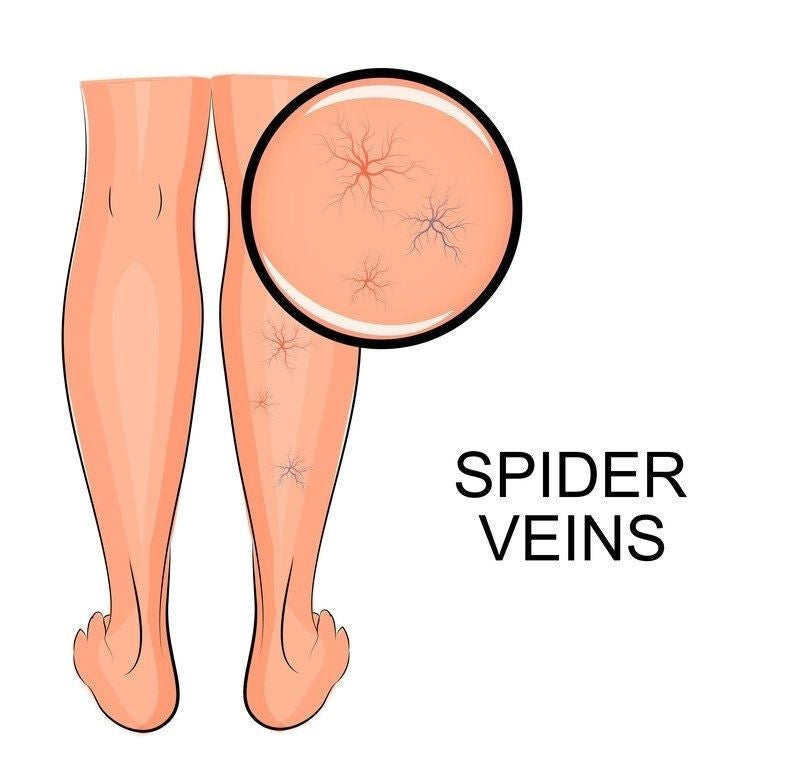
The condition in which widened venules or tiny blood vessels cause patterns or threadlike red lines is called either spider veins or telangiectasia or spider angioma or spider nevus or nevus Araneus or vascular spider. It is a collection of small, dilated arterioles (blood vessels) clustered very close to the surface of the skin. The web like the appearance of spider veins as fine clusters form gradually in the areas that are easily seen as cheeks, fingers, eyes, nose and lips. Sometimes they feel unattractive and cause discomfort. Most of people try to remove the telangiectasia and spider veins by causing damage to the vessel and forcing it to collapse or scar. Removal processes may include chemical injections for the purpose, laser treatments or compression stockings. By this removal, red marks or patterns on the skin are removed.

Causes Of Spider Vein Or Telangiectasia:
The exact cause of spider vein is unknown yet researchers believe a number of causes contributing to the development of telangiectasia. These causes may be of multiple origins as environmental, genetic or a combination of both. Most of the time its reason is considered to be chronic exposure to extreme temperatures or direct sun because they usually appear on the body when exposed to sunlight or air directly. Other causes of spider veins may include:

- Exposure to the sun: Direct exposure to the sun for long term as walking for many hours in the sun, working in the direct sun for long time may cause spider veins.
- Any injury: Any injury to the blood vessels may cause spider veins or telangiectasia which may burst after some time if not removed causing hemorrhages.
- Changes in hormonal levels: Hormones increase or decrease during a month several times like in whole life. Hormonal ups and downs may occur during puberty, monthly periodical cycles, pregnancy, menopause or nay other dietary or medications which may cause spider veins or telangiectasia.
- Any underlying illnesses: Liver diseases (chronic liver disease, liver cirrhosis either due to alcohol or without alcohol intake, enlarged liver), hypertension, diabetes, cardiac stress or any other underlying disease that may create spider veins as an outcome of the long term caused stress may be treated along with the symptoms of spider veins.
- Alcoholism: Chronic intake of alcohol may cause liver diseases as underlying cause of spider veins and may directly affect the flow of blood in vessels.
- Pregnancy: During pregnancy the weight of uterus and baby exerts large amount of pressure on venules and cause spider veins.
- Aging: Elastin fiber decreases with age while collagen increases causing weakening of blood vessels in long term and may give rise to spider veins.
- Rosacea: Enlarged venules in the face create a flushed appearance in nose and cheeks.
- Corticosteroids: Habitual use of corticosteroids for a number of reasons as obesity, cosmetic purpose, and pregnancy may thin and weakens the skin.
- Scleroderma: Scleroderma is a skin condition in which hard scales appear on the skin and may cause contraction and hardening of the skin.
- Dermatomyositis: Inflammation of the dermal skin as well as underlying muscular tissues may cause spider veins.
- Sytemic lupus erythematosus: Skin becomes extra sensitive to sunlight and extreme temperatures in systemic lupus erythematous.
- Genetic causes: Hemorrhagic telangiectasia may have hereditary causes and the affected may inherent it from at least one parent. Almost three known genes are suspected to cause telangiectasia. As a dominant gene, it takes one mutated gene to cause HHT, although it may receive one mutated gene or two mutated genes.
.
Symptoms Of Spider Veins Or Telangiectasia:
Telangiectasia are sometimes uncomfortable although they are not life-threatening because some people may not like their appearance. They develop gradually but with the use of health and beauty products may cause skin irritation. The irritant cosmetics may include sponges and abrasive soaps. The most common signs and symptoms of spider veins are:
- Vessel cluster: Appearance of a vessel cluster is the only symptom of people with spider vein. A red dot in the center of a cluster of thin vessels is the prominent symptom. The colored vessels as red, blue or purple colored ones form a web-like shape. These vessels disappear when you apply pressure and reappear as soon as blood flows back into the vessels.
- Aching or burning: Burning or aching occurs in the area of the vessel cluster which may appear on face, neck and legs (sun-exposed areas). The pain occurs when the vessels are in the legs and after long period of standing.
- Pain or aching: A sensation of pain or aching may appear due to pressure on venules.
- Itching: Extra flow of blood towards the venules or veins may create itching.
- Marks/patches: Thread/like red marks or patches appear on the skin as prominent sign or symptom.
- Nosebleeds: Frequent nosebleeds may appear as a symptom of spider veins.
- Shortness of breath: Breath shortness may appear.
- Seizures: Seizures may appear due to increased blood flow towards brain.
- Small strokes: Small strokes may appear due to incoherent blood flow.
- Birthmark: Port-wine birthmark may appear as a sign.
Treatment Options For Telangiectasia:
General appearance of skin is the treatment focus. Different methods to achieve the result are:
- Laser therapy: The widened vessels are the laser targets and are sealed by it (little pin is involved in the procedure and has short recovery period).
- Surgery: A painful procedure with long recovery time is the surgery to remove widened vessels. If your varicose veins cause a lot of pain or damages your overall health, then this invasive procedure may be tried. Vein ligation and stripping is a surgical treatment that may require anesthesia. The surgeon may cut your skins, may cut the varicose veins and may remove the incisions.
- Sclerotherapy: A chemical solution is injected to cause damage to the inner lining of the blood vessel that may cause a blood clot that collapses, scars or thickens the venule. Although no recovery is needed with this procedure, yet there may be some temporary exercise restrictions.
- Embolization: Embolization may be done to close or block a blood vessel.
Who Is At Risk Of Contracting Telangiectasia?
Telangiectasia is the most common disorder to attack even the healthier ones but most commonly it may attack specific life styles and certain people who may become prone to its attack. These may include:
Work outdoors/sun exposure:
People who work outdoors and face the extremes of temperature as well as stay under direct sunlight for more number of hours become the prime target of telangiectasia.
Sit or stand all day:
People who sit or stand for long hours and make their body at a similar position for long hours are more prone to get the attack of telangiectasia.
Misuse alcohol:
People who misuse alcohol or take extravagant amount of such a poison become prey of the spider veins most frequently.
Pregnancy:
Pregnancy plays a major role to make you prone to this disease that is spider veins due to extra burden of baby weight and uterus on the legs as well as change of hormones affect the general physiology in a negative way.
Age factor:
Elderly or older people are more likely to get telangiectasia as the skin ages. Valves in the heart get weaken by the advanced age. The older you get, the more vulnerable you become to spider nevi.
Disease factors:
Presence of underlying disease factors as dermatomyositis, systemic lupus erythematous or scleroderma or rosacea may make you prone to develop spider veins.
Corticosteroids:
Use of corticosteroids may make you prone to the spider veins causing weakness in the body.
Hormonal changes:
With everyday changes in your body with advancing age, a number of factors affecting levels of hormones as puberty, pregnancy, menopause and use of contraceptives may cause spider veins.
Family history:
Weak valve vessels and constricted arteries may have been a part of your family history so you must have double the chance to get the spider veins.
Obesity:
Excessive weight gain giving an unhealthy condition may also account for maximum chances of spider veins due to extra weight gain applying pressure on the veins of the legs.
Diagnostic Tests For Spider Veins:
Telangiectasia is easily visible from the patterns or thin threadlike red lines on the skin and doctors may rely on these clinical signs. Simply by looking at the appearance of skin in question, your physician can judge your condition if spider veins occur. The physician may have taken into account a number of factors as:
- Skin biopsy: Skin biopsy may be done to confirm the diagnosis.
- Intake of hormone supplements: Since changes in the hormones level may affect your body in general making it more prone to spider veins occurrence.
- Intake of any other medications: Interaction with any other medications may affect your skin conditions or veins in general.
- Alcohol consumption: Alcohol or any other abusive drug may have a bad effect on your liver causing weakness, debilitation and weakened arteries and veins.
- Liver diseases: Liver has important tasks in our body including detoxification of blood, food digestion, protein production helping to clot the blood etc. thus making it necessary to view its condition.
Doctors may check underlying diseases to ensure the occurrence of telangiectasia. Associated diseases may include:
Venogram: A venogram may be done to assess your veins further during which the physician may inject a special dye into your legs and may take x-rays of the area. Dye may appear on the x-ray result providing your doctor with a better view of how your blood is flowing.
Ultrasound test: An ultrasound may be done to check your flow of blood. It is a non-invasive test that may use high-frequency sound waves that may allow your doctor to see how blood is flowing in your veins.
Liver panel test: A liver panel test involves taking blood samples to test for enzymes and protein production to assess the decreased or increased levels of these substances etc.
Osler-Weber-Rendu Syndrome:
It is also called HHT, which is an inherited disorder of the blood vessels in internal organs and skin that may cause excessive bleeding.
Sturge-Weber disease:
It is a rare disorder that may cause a port-wine stain birthmark and other nervous problems.
Spider angiomas:
An abnormal collection of blood vessels near the surface of the skin is called spider angiomas.
Xeroderma pigmentosum:
A rare condition in which skin and eyes become extremely sensitive to ultraviolet light is xeroderma pigmentosum.
Arteriovenous malformations (AVMs):
Formation of abnormal blood vessels may be caused by the HHT which may appear in several areas of the body. These allow direct connections between arteries and veins without intervining capillaries. It may cause deadly hemorrhage in brain, liver or lungs.
Prevention Of Telangiectasia:
At the first step, you always must avoid any exposure to sun or heat for a long time since they may cause permanent damage to the veins. You may prevent the occurrence of spider veins by following certain measures:
- Avoiding hormone therapy: You must avoid hormonal supplements or extra intake of hormones to avoid the changes in liver and other places to avoid occurrence of spider veins.
- Wearing sunscreen: Try to wear sunscreen on your skin and other parts of body that are exposed to avoid the direct effect of sun or heat. The commonly affected areas may be face, neck, hands, feet and face etc.
- Avoid unnecessary medications: Avoid any unnecessary medication that may prompt spider veins by long-term use disturbing your normal physiology.
- Treat liver disease if present: Treat any underlying disease especially liver disease if present so that normal physiology may not exceed the limit.
- Alcohol and stimulating food: Avoid such food that may stimulate the action potential and flow of blood towards the veins thus activating the nerves unnecessarily causing constriction or edema. Avoid alcohol overconsumption.
- Decrease obesity: Try to decrease weight to overcome the underlying issues.
- Exercise regularly: Do exercise regularly to maintain a healthy life style to improve your blood circulation.
- Compression stocks: Use stockings or compression socks to avoid spider veins. The stockings may place enough pressure on your legs so that blood may flow easily to your heart. These may help to decrease swelling.
Reasons Of Broken Blood Vessels On Your Face:
Dilated or enlarged blood vessels also called spider veins occur just beneath your skin’s surface. Small, red lines spread out into a web-shaped form due to these broken blood vessels. These can develop on anywhere on the body but they are most common on the face and legs. Spider veins are easily treatable once the underlying reason is figured out properly. The broken blood vessels may appear at any age ranging from childhood to adult including small children. The common causes of broken blood vessels may be:
- Genetics and hereditary: Spider veins tend to run in families due to a number of unknown reasons. Individual risk factors increase with advancement in age.
- Gestation: Estrogen hormones increase during gestation time and may lead to broken blood vessels. Pregnancy-related spider veins heal on their own postpartum. Skin changes are a part of pregnancy.
- Rosacea: Excessive redness and flushing occurs during rosacea. Broken blood vessels are common in erythematous telangiectasia rosacea.
- Sun exposure: Blood vessels become enlarged by excessive sun exposure. If you get a sunburn, some of the blood vessels in your face may become noticeable by peeling off of the top layer of skin.
- Changes in weather: Extreme increase in temperature may cause blood vessel dilation.
- Chemical or environmental irritants: Irritants present in the environment and near or inside factories may cause spider veins.
- Alcohol consumption: Occasional or moderate alcohol consumption may cause flushed skin due to enlarged blood vessels. Heavy alcohol use or binge drinking may lead to spider veins.
- Injuries: Bruising may occur due to minor or significant injuries. Broken blood vessels may become noticeable with bruises on your face.
- Sneezing or vomiting: A violent sneeze or a vomit spell can cause extreme pressure in your face causing broken blood vessels in face or skin.
How Are They Diagnosed?
It’s easy to diagnose and identify the broken blood vessels but still you may need confirmation from doctors. An outpatient care solution or prescription medication may be recommended by your doctors in the case of numerous spider veins. The underlying diseases or problems may account for a separate treatment plan for the management of spider veins, e.g. the underlying health conditions like rosacea.
Natural Remedies For Broken Blood Vessels:
Natural remedies come as the first line of treatment for broken blood vessels on the face. Unless you have the sensitivity to any of the ingredients, natural treatments are considered safe from any significant risks. You must try at-home remedies for broken blood vessels. Some of these may be:
Apple cider vinegar: The redness and swollen appearance of spider veins may be managed and lessened by the use of common pantry staple. In the place of your daily toner or astringent, vinegar may be used and applied with a cotton ball.
Horse chestnut: It is a natural herb used for a variety of skin ailments. Some of the people may use it for vein health too. Either as a supplement or in the topical forms, the horse chestnut may be used safely for the treatment of spider veins. The preparations made from bars must be used and applied on face directly.
Use of warm water for face only: Heat can easily cause broken blood vessels and if you want to take warm water, make it sure that it is not hot bath, rather warm showers and baths may be tried. Always wash your face gently even with warm water.
Medical Treatments For Broken Blood Vessels In Face:
Natural remedies may ameliorate your symptoms in a limited fashion but when it stops working you may try the remedies and treatments that are recommended by your physician. Among the available options are:
Retinoids: Topical creams, especially those with retinoids work by removing the outermost layer of the skin. These topical applications may help to reduce the appearance of spider veins. These components are used majorly for acne and rosacea.
Laser therapy: This therapy works by making spider veins fade completely by destroying the poor functioning veins. This therapy may use strong laser lights.
Intense pulsed light: The deeper penetrating light that may reach the second layer of skin without harming the top layer is the intense pulsed light. The concept is same as the laser light but with deep penetration.
Sclerotherapy: This is an injection-based therapy that may help spider veins to move away within few weeks. The physician may inject a solution into broken blood vessels during the procedure that may help to close the broken blood vessels. The blood as a result may be rerouted to unnoticeable vessels.
The laser treatments and other surgical procedures may be carried ouit with the help of a professional expert since the side effects may cause redness, itching and scarring.
Can Broken Blood Vessels In Face Be Prevented?
Natural remedies may be used as a priority to prevent and treat broken blood vessels but you must consider preventive measures to avoid spider veins at first place. If you are currently undergoing treatment for spider veins or rosacea, then stick with your plans if you don’t see any improvement. You may follow certain preventive measures to prevent spider veins on your face by following these rules:
Reduce sun exposure: Especially during peak hours of noon and weather of summer, wear sunscreen every day for your skin protection. This may be especially important if you live in the areas near equator.
Avoid extreme heat: Extreme heat exposures from any areas as spas, saunas and weather extremities may call for an increase in blood vessel dilations.
Take moderate amount of alcohol, if necessary: This must be confirmed from your physician if you plan to quit alcohol intake and need assistance for that or if you must take only limited amount.
Wearing protective gear: Always use face gear and helmets for cycling, sports and other physical exercises that may help to reduce the injuries and related spider veins.
Avoiding hormone therapy: You must avoid hormonal supplements or extra intake of hormones to avoid the changes in liver and other places to avoid occurrence of spider veins.
Chemical or environmental irritants: Irritants present in the environment and near or inside factories may cause spider veins, so always cover your face while working or passing by any such area.
Injuries: Bruising may occur due to minor or significant injuries. Broken blood vessels may become noticeable with bruises on your face. Try to protect your face as a priority.
Sneezing or vomiting: A violent sneeze or a vomit spell can cause extreme pressure in your face causing broken blood vessels in face or skin. Try to reduce the pressure on face always.
Decrease obesity: Try to decrease weight to overcome the underlying issues. Double chin or extra skin on face may cause dilation of blood vessels.
Exercise regularly: Do exercise regularly to maintain a healthy life style to improve your blood circulation.