Gingivitis does not crash into your life loudly, it slides in quietly. A little bleeding when you brush, a tender spot along the gums, a strange taste in your mouth, and suddenly there is a discomfort you cannot ignore. That subtle shift is often the earliest sign that something has changed inside your gums. At first, it feels minor. But beneath the surface, bacteria start building a pattern that can rapidly grow into something far more damaging.
This is why understanding what are the stages of gingivitis matters so much. When you know how it starts, how it progresses, and how it behaves, you can stop it long before it turns into a bigger, more expensive, more painful problem.
Most people recognize gingivitis only when it becomes uncomfortable, but catching it earlier makes everything easier. That is the point of this guide, to walk you through the stages with clarity and confidence, and to help you take meaningful action before things escalate.
By the end of this article, you will understand what each stage looks like, how it feels, how fast it moves, and what you can do right now to protect your gums with practical, realistic steps, including natural daily care options that can support your oral health long term.
The First Stage of Gum Disease - Gingivitis!

When people search what are the stages of gingivitis, they usually want a clear explanation of how gum disease actually begins. Gingivitis is the earliest point in that journey, and fortunately, the most treatable stage. It starts with something incredibly ordinary, plaque. This sticky bacterial film forms on your teeth every day from food, saliva, and leftover debris. If it is not cleaned properly, it starts irritating the gums right where the teeth meet the soft tissue.
The Early Changes You Might Miss
Gingivitis begins so quietly that most people ignore it. The gumline becomes slightly swollen, the color shifts from a healthy pink to a deeper red, and brushing might feel a bit uncomfortable. These tiny changes are your body’s first reaction to bacterial irritation. Even mild bad breath can be a sign that the bacteria are lingering longer than they should.
How Gingivitis Behaves in the Beginning
During the early phase, gingivitis stays near the gumline. No deep pockets have formed yet. The bone is not affected. Nothing irreversible has happened. This stage is mainly about inflammation triggered by bacterial buildup. If someone improves their oral routine at this point, the gums can bounce back quickly.
Why Early Detection Is So Important
People often underestimate this stage because the symptoms feel small. But the truth is, early gingivitis is the turning point. This is when gum disease can still be controlled with consistent brushing, flossing, and targeted oral care solutions. Once plaque hardens into tartar, however, removal becomes more difficult and the inflammation gets worse.
Understanding this first stage gives you an important advantage. You now know what the warning signs look like, and that awareness alone can help you stop the progression before it becomes something more serious.
Why Gingivitis Occurs, The Real Triggers Behind the Condition

To understand what are the stages of gingivitis, you first need to understand what pushes your gums into trouble in the first place. Gingivitis has several causes, and the mix of these factors determines how fast the condition develops. Although plaque is the primary trigger, other lifestyle and health elements make your gums more vulnerable than you might expect.
The Daily Habits That Start the Problem
Poor brushing and flossing are the most common causes. When plaque stays on the teeth for too long, it becomes tartar, a hardened substance that traps bacteria along the gumline. This buildup irritates the gums, leading to swelling and bleeding. Even skipping flossing for a few days can create the perfect environment for bacteria to thrive.
Lifestyle Choices That Speed Things Up
Smoking is one of the biggest accelerators of gingivitis. It restricts blood flow, weakens gum tissue, and makes healing much harder. Your body cannot fight infection as effectively when exposed to tobacco, making plaque more damaging. Stress, lack of sleep, and poor nutrition also weaken your immune response and allow inflammation to grow faster.
Natural Body Changes That Increase Gum Sensitivity
Hormonal shifts during puberty, pregnancy, or menopause change how gums react to plaque. These changes can make your gums more sensitive and prone to swelling. Even if your brushing routine stays the same, the hormonal fluctuation can intensify gum irritation.
Medical Conditions That Make Gingivitis More Likely
Conditions like diabetes reduce the body’s ability to fight infection. Some medications cause dry mouth, removing saliva’s natural cleaning effect. With less moisture in the mouth, plaque forms faster, making gingivitis much easier to develop.
Knowing these risk factors helps you understand why gingivitis happens and how you can control or prevent it before it progresses through the next stages.
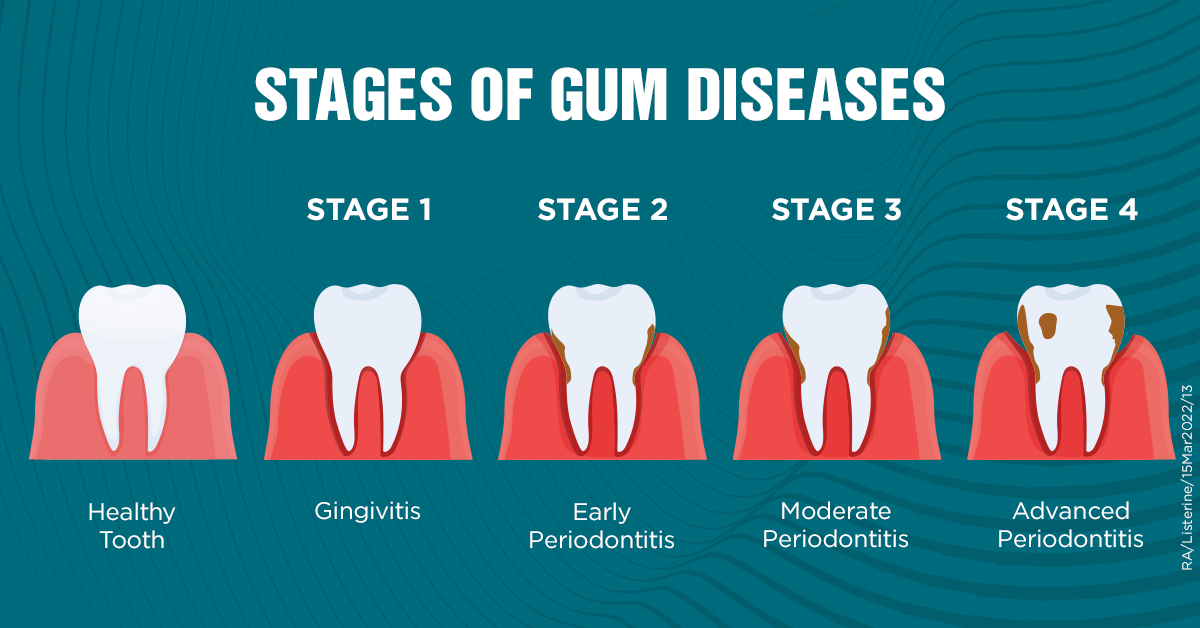
What Are the Stages of Gingivitis, A Detailed Breakdown of How It Progresses

Gingivitis does not progress randomly. There is a clear pattern. When people search what are the stages of gingivitis, they want clarity, not vague descriptions. So here is the full breakdown, explained step by step so you can recognize exactly where you or someone else might be on the gum disease spectrum.
Stage 1: Initial Gingivitis, Where Inflammation Begins
This is the starting point. In this stage, bacteria sit right along the gumline. The plaque layer is still soft. The gums appear slightly red and may bleed during brushing or flossing. Pain is minimal, and there is no permanent damage yet.
Key indicators include:
-
Mild swelling.
-
Slight sensitivity when brushing.
-
Occasional bleeding.
-
A change from bright pink gums to a darker shade.
At this stage, the gums can recover quickly with better oral hygiene, routine flossing, and the introduction of targeted natural care products.
Stage 2: Mild Gingivitis, Where Plaque Starts Hardening
As bacteria stay longer on the gumline, plaque begins to harden into tartar. Once tartar develops, brushing alone cannot remove it. This buildup creates irritation around the gums and increases inflammation.
Signs become more noticeable:
-
Gum tenderness.
-
Consistent bleeding during brushing.
-
Lingering bad breath.
-
Slight recession starting around the teeth.
This is still reversible, but it requires more attention and likely a professional cleaning.
Stage 3: Moderate Gingivitis, Where Inflammation Spreads Deeper
This is the point where many people begin to worry. The inflammation becomes more visible, and the swelling intensifies. Plaque and tartar now extend further under the gumline.
Changes include:
-
Deeper red coloration.
-
More obvious swelling.
-
Development of early gum pockets.
-
Discomfort when chewing or brushing certain teeth.
The early gum pockets are significant. They show that inflammation is now affecting the space between gums and teeth. Without proper care, this stage can tip into early periodontitis.
Stage 4: Advanced Gingivitis, The Last Stage Before Periodontitis
At this point, symptoms are much harder to ignore. The gums may feel sore, bleeding becomes regular, pockets deepen, and there may be pus or a foul taste in the mouth.
Possible indicators:
Visible gum recession.-
Loose feeling in some teeth.
-
Increased sensitivity.
-
More severe bad breath.
-
Larger pockets around the teeth.
This stage is the bridge between gingivitis and periodontitis. While the bone is not yet damaged, the gums are extremely vulnerable. Immediate intervention is necessary to avoid irreversible harm.
Understanding these stages helps you identify problems early, respond faster, and prevent the condition from becoming something more advanced and more expensive to treat.
Progression, Severity, And Speed: Not All Gingivitis Is the Same
It’s not just about stages. How fast gingivitis progresses can vary, and dental professionals use grading systems and severity levels to talk about it.
-
Grades of Progression: Some people have Grade A (slow), Grade B (moderate), or Grade C (rapid) progression.
-
Severity and Complexity: Once gingivitis shifts into periodontitis, clinicians assess things like bone loss, tooth mobility, pocket depth, and more.
-
Staging of Periodontitis: After gingivitis, periodontitis is commonly divided into Stage I, II, III, and IV based on how much damage there is.
So when you ask, what are the stages of gingivitis, keep in mind: it’s not just a linear climb. Where you are on that climb depends on your habits, health, and how quickly your gums are responding.
Why Does It Matter? What Are The Risks of Not Treating Gingivitis
You might think, “It’s just bleeding a little… no big deal.” But ignoring what are the stages of gingivitis is risky. Here’s why:
Progression to Periodontitis: Untreated gingivitis can lead to irreversible damage, like bone loss and gum recession.
Systemic Health Risks: Gum disease links to other health issues; heart disease, diabetes complications, and respiratory infections, for example.
Tooth Loss: Later-stage gum disease (periodontitis) can cause loose teeth, shifting teeth, or even tooth loss.
Quality of Life: Bad breath, pain, sensitivity; these affect how you eat, talk, and feel confident.
That’s why answering what are the stages of gingivitis isn’t just academic. It’s a wake-up call.
How to Diagnose the Stages, What Dentists Look For?
When it comes to gum health, most people assume a dentist simply “looks at your gums” and instantly knows what’s going on. In reality, diagnosing gingivitis and the early stages of gum disease is a structured, detailed process.
Dentists rely on multiple clinical cues, measurements, and visual markers to map exactly where your gums fall on the inflammation spectrum, from healthy, to mildly irritated, to the earliest shifts toward periodontal disease.
Below is a deeper breakdown of what really happens during an evaluation.
1. The Visual Examination, First Signs That Something’s Off
Before any instruments are used, your dentist visually inspects the gum tissues. They look for:
Color changes (healthy coral pink vs. red or bluish tones).
Shiny or swollen surfaces.
Gum margins that appear “puffy” or rolled.
Areas where plaque accumulates more heavily.
Any recession points where the gum has pulled slightly away from the tooth.
This initial step already gives clues about the stage you're in, especially if the gums appear irritated before probing even begins.
2. Gum Probing, Measuring Pocket Depths
This is one of the most important diagnostic tools. A periodontal probe measures the sulcus depth around each tooth:
1–3 mm: Normal, healthy range.
4 mm: Early warning sign.
5–6 mm: Early-to-moderate periodontal involvement.
7 mm or more: Advanced periodontitis.
The dentist checks multiple points around each tooth, not just one, because inflammation doesn’t occur uniformly. These numbers help determine if your condition is still gingivitis (no bone loss) or if the disease has already progressed.
3. Bleeding Index, A Marker of Active Inflammation
Bleeding on probing tells the dentist your gums are actively inflamed. Even a small amount of bleeding, especially in multiple areas, indicates the immune system is responding to bacteria trapped under the gumline.
No bleeding: Healthy or well-controlled gums.
Localized bleeding: Usually mild gingivitis.
Generalized bleeding: Moderate to severe gingivitis or early periodontitis.
This is one of the clearest indicators of where you stand.
4. X-rays and Bone Analysis
Gingivitis does not show bone loss, but early gum disease does. That’s why dentists use X-rays to:
Detect bone height around each tooth.
Identify early crestal bone loss.
Check for tartar deposits under the gumline.
Evaluate root surfaces.
This is key because even if your gums look slightly inflamed, unnoticed bone loss means you're no longer in the gingivitis stage.
5. Plaque and Tartar Mapping
Dentists also check:
How much plaque is present.
Whether tartar has formed above or below the gumline.
Which teeth or areas are more prone to buildup.
This mapping helps create a personalized treatment plan and determines whether you simply need improved home care or require scaling/root planing.
6. Final Stage Determination
Combining all the above data, the dentist assigns your gum health to a specific stage:
Stage 0: Healthy gums.
Stage 1: Mild gingivitis.
Stage 2: Moderate gingivitis.
Stage 3: Early periodontitis.
Stage 4: Moderate/advanced periodontitis.
This structured approach ensures that treatment is accurate and tailored, not just guesswork.
How to Treat Each Stage, What You Can Do at Every Level of Gingivitis

People searching what are the stages of gingivitis also want to know what to do at each stage. Treatment depends on how far along the inflammation has progressed. The earlier you act, the easier it is to reverse the condition.
Treating Stage 1: Initial Gingivitis
At this early stage, simple improvements work extremely well. Brushing twice daily with a soft toothbrush, flossing regularly, and using a natural antimicrobial rinse can reduce inflammation quickly. Most people see improvement within one to two weeks.
Adding an oral solution like The Goodbye Company Gum Disease product can help soothe irritation and support gum healing.
Treating Stage 2: Mild Gingivitis
By this stage, plaque may have hardened into tartar. Professional cleaning is usually needed. Your dentist will remove the buildup from around the gumline. At home, you should strengthen your brushing technique and use an oral care routine that focuses on reducing bacteria.
This is also when consistent use of natural oils like clove, neem, and omega-rich blends can help calm inflammation between appointments.
Treating Stage 3: Moderate Gingivitis
Since gum pockets may be forming, you need deeper cleaning. Dentists perform scaling and root planing to remove tartar under the gums. This helps reduce pocket depth and allows the gums to reattach.
Home care becomes extremely important here. Daily use of an anti-inflammatory, antibacterial oil like The Goodbye Company Gum Disease oral solution can help support the healing process and limit new bacterial buildup.
Treating Stage 4: Advanced Gingivitis
At this point, the gums are extremely inflamed. Professional treatment is required. Some people may need advanced cleanings, medicated rinses, or specific periodontal therapies. Once the infection begins moving deeper, the goal is to stabilize the gums.
At home, keeping the area clean becomes a daily priority. Using gentle, natural oils can help soothe the gums and fight bacterial growth while the dental treatments address the deeper issues.
A Natural, Preventative Approach, The Goodbye Company Solution
Alright, so you know what are the stages of gingivitis, now, how do you prevent or treat it in a natural way? Let me introduce something powerful: The Goodbye Company Gum Disease oral solution.
Why This Solution Stands Out
-
It’s all-natural, made with omega-3 and omega-9 oils infused with neem and clove essential oils. These ingredients are not just gentle, they’re effective.
-
Omega-3 and 9 oils help reduce inflammation. Neem is known for its antibacterial properties. Clove is a classic for dental health, helping soothe and fight germs.
-
This solution is designed to help both prevent and treat gingivitis, not just mask the symptoms.
When It Makes a Difference
If you’re already dealing with signs like bleeding gums, tooth sensitivity, or bad breath, incorporating this oral solution into your daily oral care routine can make a real difference. Over time, it helps support gum healing, keeps bacterial growth in check, and strengthens your gums naturally.
By using this product alongside brushing, flossing, and regular dental checkups, you’re giving your mouth a powerful, nature-based line of defense. It's not a quick fix, it’s a sustainable, science-backed way to help keep gingivitis in check.
Preventing Progression, Simple Habits That Help
Stopping gingivitis from progressing isn’t about buying fancy products or committing to a complicated routine. It’s about building consistent habits that protect your gums day after day. Even small, simple actions, done regularly, can stop inflammation in its tracks and support your body’s natural healing ability.
Below are habit expansions that go deeper into why these steps matter and how they block the progression to more serious gum disease.
1. Mastering Proper Brushing, Technique Over Force
Brushing twice a day is essential, but how you brush matters even more:
-
Use soft bristles to avoid scratching or irritating your gums.
-
Keep your brush at a 45-degree angle, sweeping gently into the gumline.
-
Spend at least 2 minutes each session, ensuring full coverage.
-
Replace your toothbrush every 60–90 days.
This routine removes plaque before it hardens and helps prevent the earliest signs of gingivitis.
2. Flossing and Interdental Cleaning, Where Your Brush Can’t Reach
Plaque loves tight spaces between teeth, areas your toothbrush can’t access. That’s where flossing steps in:
-
Use traditional floss, interdental brushes, or floss picks.
-
Slide gently, avoiding snapping motions.
-
Focus on each tooth’s natural curve.
Regular interdental cleaning disrupts bacterial colonies, preventing them from triggering inflammation.
3. Rinse Wisely, Support the Healing Environment
An antimicrobial or natural rinse helps flush away lingering bacteria:
-
Natural options (like The Goodbye Company solution) help reduce inflammation gently.
-
Rinsing reaches deeper areas of the gumline, where bristles and floss might miss.
-
It reinforces a cleaner oral environment after brushing.
Think of it as an extra layer of defense.
4. Monitor Your Risk Factors, Manage What You Can
Certain habits and health conditions directly impact gum health:
-
Smoking reduces blood flow to the gums, slowing healing.
-
Diabetes affects the body’s ability to fight infection.
-
Chronic stress elevates inflammatory responses.
-
Hormonal changes (especially in women) increase gum sensitivity.
By managing these factors, you reduce the burden on your gums and allow them to stabilize.
5. Commit to Regular Dental Cleanings, Prevention Beats Repair
Professional cleanings are non-negotiable if you're dealing with gum inflammation:
-
Dentists remove tartar you can’t reach.
-
They monitor early changes before they worsen.
-
They guide you on technique and habits.
Skipping cleanings often leads to plaque hardening into tartar, which accelerates gum disease.
6. Nourish Your Body, Diet Shapes Gum Health
A balanced diet helps your gums stay resilient:
-
Reduce sugary snacks to starve harmful bacteria.
-
Eat vitamin-rich foods (C, D, and K2) that support gum integrity.
-
Choose mineral-rich whole foods to strengthen tooth structure.
-
Drink more water to support saliva production, nature’s natural cleanser.
Your mouth is part of your body’s immune system. A healthy diet means stronger defenses.
7. Consistency Is Everything
The real secret to preventing progression is consistency. Not perfection, just showing up every day with small, protective habits that add up over time. When you combine smart daily care with a targeted natural gum solution, you create a powerful environment where gingivitis struggles to survive.
FAQS - What Are the Stages of Gingivitis
Let’s tackle some of the most frequently Googled questions around what are the stages of gingivitis, because these are the things people really worry about.
How long does it take for gingivitis to turn into periodontitis?
It varies a lot. Some sources suggest progression from gingivitis to early periodontitis can happen in a few months, while others say it could take longer or never happen, depending on factors like oral care, health, and genetics.
Can gingivitis go away on its own?
It can, if treated properly. At Stage 1, when symptoms are still mild, improving your brushing, flossing, and professional cleanings can reverse damage. But if you ignore it, it could worsen.
What does stage 1 gingivitis look like?
In stage 1, your gums might look slightly red or puffy. Bleeding may occur during brushing or flossing. There’s often bad breath, but you probably won’t feel pain.
Is bleeding gums always gingivitis?
Not always, but bleeding gums are a very common sign. Other issues (like trauma, aggressive brushing, or certain medical conditions) can also cause bleeding. If it’s coupled with swelling or bad breath, it’s more likely to be gingivitis.
Can gingivitis cause tooth loss?
By itself, gingivitis doesn’t usually cause tooth loss. But if it progresses into periodontitis, where gum pockets deepen, bone is lost, and support structures weaken, then yes, tooth loss becomes a risk.
Final Word
Let’s circle back: what are the stages of gingivitis? There are clearly defined stages, from mild, reversible inflammation to moderate buildup and finally to advanced, damaging disease that can lead to periodontitis. Knowing those stages means you can catch trouble early.
Here’s your action plan:
-
Pay attention to your gums, are they bleeding, swollen, or sensitive?
-
Get a proper dental checkup and ask your dentist to assess your gum health and staging.Adopt strong oral care habits, including brushing, flossing, and using a natural solution like The Goodbye Company Gum Disease oral solution.
-
Stick with it, gum health takes consistency.
By doing this, you’re not just treating symptoms. You’re actively preventing your gingivitis from progressing into something much worse. And the Goodbye Company oral solution offers a natural, effective addition to your daily routine, helping reduce inflammation and support healing without harsh chemicals.