Many people ignore bleeding gums and mild oral discomfort, assuming it's just a temporary issue. But oral health isn’t confined to your teeth and gums, it’s deeply connected to your immune system, your blood, and even your lymphatic system.
If you’re wondering “can gingivitis cause swollen lymph nodes?” - sadly, the answer is yes, but there’s a lot more you need to know.
Why You Should Take Gingivitis Seriously?
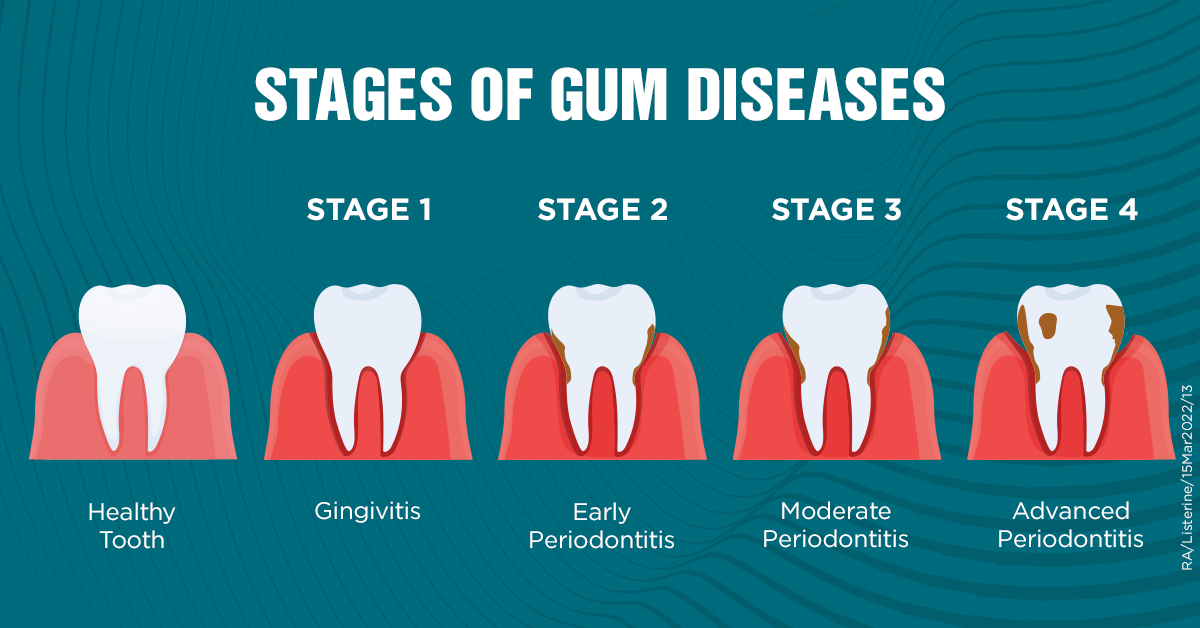
The primary and mildest gum disease is gingivitis, which usually occurs when sticky plaque of bacteria gathers on your gum line and teeth. It may begin without warning: you may see your gums bleed slightly whenever you brush or floss. Perhaps, you have a bad breath even with proper hygiene. Most people don’t bat an eye towards these symptoms.
The thing is though, when you do not pay attention to gingivitis, it can turn into periodontitis, which is a serious problem that destroys your gums, bones, interconnective tissues that keep your teeth securely in place.
What Are Lymph Nodes And Why Do They Swell?
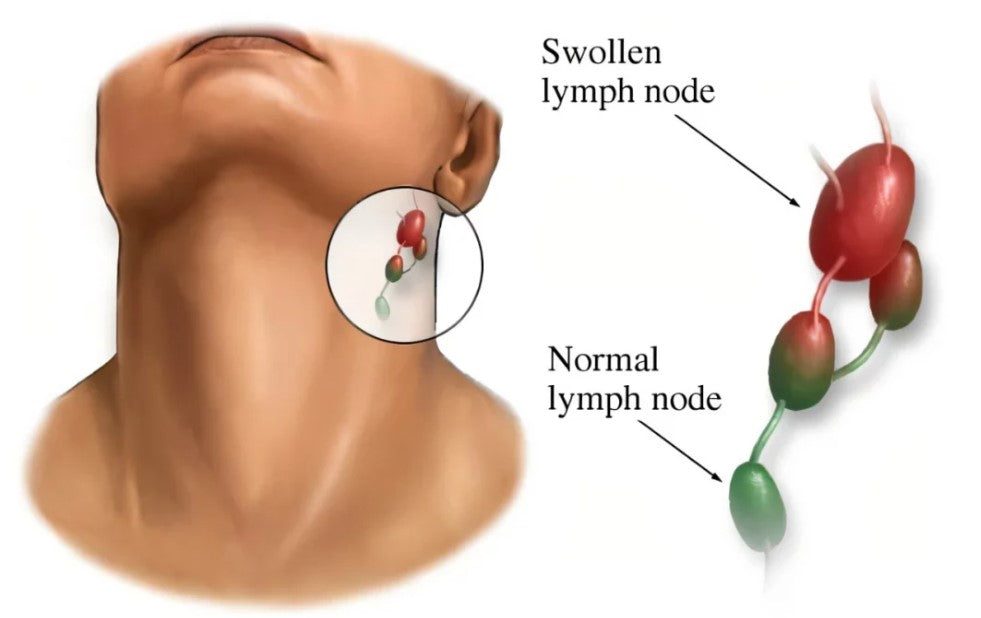
Lymph nodes are small, bean-shaped structures that filter out harmful substances. They play an important role in your lymphatic system, along with lymph fluid, lymph vessels, and other organs that aids your body in the fight against infection and keeping the body fluid levels as balanced as possible. These nodes are filled with immune cells known as lymphocytes which wipe out and kill bacteria, viruses, and other foreign agents.

How Do Lymph Nodes Function?
Lymph nodes clean the lymphatic fluid that contains waste products, germs and debris of dead cellular parts of the body. When either an infection or injury happens, the closest lymph nodes tend to swell as they increase the activity in the immune system. This swelling is caused by multiplication of lymph cells and accumulation of fluids as the node tries to trap and neutralize the threat.
Why Swelling Happens
Lymph node enlargement - also called lymphadenopathy; is normally an indication of your immune system getting overworked. That is how your body tells you that it is reacting to something out of the ordinary like maybe an infection or inflammation. If it happens to be gingivitis, nearby lymph nodes such as those under the jaw or in the neck area may become enlarged as part of this immune response.
So, the next time you feel tenderness or swelling around your neck or jawline, it might not just be "nothing." It could be a signal that your gums, and your immune system - are under stress.?
The Link Between Oral Infections And Lymphatic Response
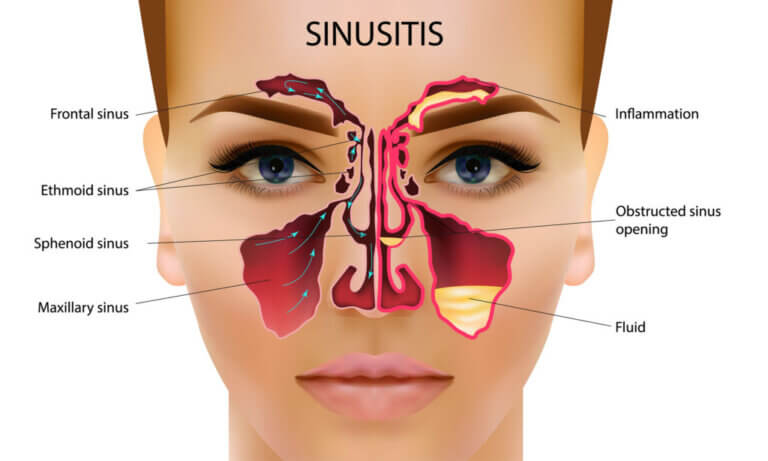
Your mouth isn’t isolated from the rest of your body. This is because your gum is a vascular tissue that is highly vascularised making it susceptible to bacteria moving into the blood or lymph nodes, in case of untreated gingivitis. This will cause the lymph nodes near you, particularly those in the neck and under your jaw - to swell and be tender.
That is your immune system at work: Catching and killing the evil microbes before they extend themselves any further.

How Bacteria Travel from Mouth to Lymph Nodes
When plaque collects on the sides of your gum line and fails to get appropriate cleaning, it generates a breeding location to bacteria. These germs are able to enter the gum and get inside your body, ranging into very small blood vessels with paths to every part of your body. The lymphatic system as an immune highway identifies this presence of bacteria and responds in turn. This incorporates induction of immune cells to the space of contamination and straining the harmful microorganism into adjoining lymph nodes. It is at that time when you start experiencing swelling or tenderness.
Why the Neck and Jaw Nodes Are the First to Swell
Since the lymphatic system drains specific areas of your body into any of the closest lymph nodes, infections in your mouth are most likely to reach the submandibular and cervical lymph nodes - the ones found under the jaw and around the neck. Such nodes come as a first line of action against oral infections.
When you experience pain and swelling in these parts during a gum contamination, it is not by coincidence. All these symptoms are telling you that there is a silent war going on in your mouth.
So, Can Gingivitis Cause Swollen Lymph Nodes? Absolutely!
When plaque buildup leads to bacterial overgrowth, your immune system detects the threat and springs into action. This immune response often includes inflammation and swelling of the lymph nodes near the affected area. If the gingivitis becomes more severe or spreads, this reaction becomes more noticeable.

The Immune Chain Reaction
Once your gums become inflamed due to gingivitis, the local immune response kicks in. Your body deploys white blood cells to fight off the bacterial invasion. This microbial war doesn’t stay local, the inflammation can travel via the lymphatic system. Your nearby lymph nodes, especially the submandibular and cervical nodes, are the first to react.
These nodes act like immune hubs. As more immune cells gather to neutralize the bacteria, the nodes themselves can become enlarged and sensitive. This enlargement is the result of increased activity - not just swelling for the sake of it. It's a physical sign that your immune system is actively working.
It's Not Always Gingivitis - But Often It Is
But here’s the nuance: swollen lymph nodes aren’t always directly caused by gingivitis alone. They usually indicate that an infection is brewing or spreading, and gingivitis, if neglected, can certainly be that source. However, they can also be tied to viral illnesses, other bacterial infections, or autoimmune flare-ups.
Still, if you're already experiencing signs of gum inflammation, like bleeding, pain, or persistent bad breath - paired with swollen nodes, it's safe to say your body is raising a flag. This section isn't just about answering the question; it's about understanding the broader implications. When your lymph nodes swell, your immune system is communicating with you. Are you listening?
Other Symptoms You Might Notice Alongside Swollen Lymph Nodes
If swollen lymph nodes are the red warning light, what other signs might accompany them?
- Bleeding gums when brushing or flossing.
- Gum tenderness or redness.
- Bad breath or metallic taste.
- Gum recession.
- Tooth sensitivity (especially to hot or cold).
- Pain when chewing.
- General feeling of malaise or mild fever.
When these symptoms occur together, your body is urging you to take action.
When Swollen Lymph Nodes Point to a Larger Problem?
Swollen lymph nodes can be harmless or a sign of something more serious. If your lymph nodes remain swollen for more than two weeks, are hard to the touch, or grow rapidly, it may indicate:
- A deep-seated tooth abscess.
- Progression of gum disease to periodontitis.
- A systemic infection.
- Autoimmune conditions.
- In rare cases, lymphoma or leukemia.
Common Causes of Swollen Lymph Nodes
|
Cause |
Location of Swelling |
Accompanied By |
Severity |
|
Gingivitis |
Under jaw/neck |
Bleeding gums, bad breath |
Mild to moderate |
|
Viral Infection (e.g. cold) |
Neck, behind ears |
Runny nose, sore throat |
Mild |
|
Bacterial Infection (e.g. strep) |
Neck, under jaw |
Fever, white patches in throat |
Moderate to severe |
|
Tooth Abscess |
Jaw, cheeks |
Severe pain, swelling, fever |
Severe |
|
Autoimmune Disorders |
Multiple locations |
Joint pain, fatigue |
Varies |
|
Cancer (rare) |
Hard nodes, fixed position |
Weight loss, night sweats |
Needs medical eval |
Can gingivitis cause swollen lymph nodes? As you can see, it’s among the leading mild-to-moderate causes of lymph node swelling localized around the jaw and neck area.
How to Manage Gingivitis Before It Escalates
Early control of gingivitis is the key to avoiding the complications such as enlargement of lymph nodes, loss of teeth and inflammation. The following are some detailed actions that you may undertake to take back the control on your oral health before the issue develops into something worse.
Step 1: Adopt an Effective Oral Hygiene Routine
Staying consistent is very important. The next thing is being consistent. Make it a habit of brushing with a medium bristled toothbrush a minimum of twice each day. Do not be in a hurry, do it slowly. Each session should last a minimum of two minutes and carry out brushing without missing any parts, mainly the gum line. Applying fluoride on the teeth can assist in building your enamel, which also prevents the formation of plaque.
Flossing is also very important. Most of you ditch it, but one daily session at flossing can get rid of the food leftovers and plaque stuck between your teeth. Failure to do so will allow the bacteria to have an ideal environment to thrive in, and increase the chances of inflammation.
Step 2: Use Mouthwash Wisely
Do not use alcohol based mouthwashes that make the already sensitive gums get irritated. Rather, apply the natural free-alcohol formula, containing only soothing, anti-inflammatory agents, such as aloe vera or essential oils. These not only clean up your mouth but they also assist in plowing down the burden of bacteria.
Step 3: Keep Your Diet in Check
Gingivitis-causing bacteria survive on sugar. Try to limit the number of sugary and starchy foods that you consume, particularly the snack foods that stick to your teeth. If possible, add more high-fiber food like fruits and vegetables, which cleanse your teeth naturally as you chew them and actually stimulates healthy saliva outflow.
Step 4: Hydrate for Oral Health
Water is important to oral health. Water cleans off food debris and neutralises the acids created by the bacteria in the mouth. It also moisturizes the mouth, which is vital in avoiding the growth of bacteria.
Step 5: Don’t Skip the Dentist
It’s easy to delay dental visits, especially if you’re not in pain. But regular checkups, ideally every six months - are crucial for early detection of gum issues. Your dentist can remove hardened plaque (tartar), which you can’t tackle with brushing alone. They’ll also monitor for signs of gingivitis or more severe periodontal problems.
By following these steps and taking gum health seriously, you’re doing more than just protecting your teeth; you’re strengthening your immune response and lowering your risk for swollen lymph nodes triggered by oral infections. Proactivity now can save you from discomfort and costly treatments down the line.
Most Important Step: The Role of Natural Anti-Inflammatories in Gum Health
Conventional oral care products can be harsh on the gums and sometimes do more harm than good. Natural alternatives are gaining popularity due to their efficacy and gentler approach.
Ingredients like neem and clove essential oils are known for their antimicrobial and anti-inflammatory properties. Neem helps reduce plaque buildup, while clove oil is a time-tested remedy for gum pain and bacterial infection. Combine that with Omega 3 and 9 fatty acids, which are scientifically proven to reduce inflammation, and you get a synergistic solution to combat gum disease from the root.
If you’re currently dealing with bleeding gums, pain while brushing, or temperature sensitivity, consider integrating a natural, oil-based oral care product into your daily routine. The right formulation can significantly reduce symptoms, control bacteria, and promote overall oral health. Many users describe such blends as the best natural gum disease cure they’ve ever tried.
When to See a Dentist or Doctor About Swollen Lymph Nodes?
While most gum-related lymph node swelling resolves with better oral hygiene, here’s when to seek professional care:
- Swelling persists beyond 2 weeks.
- Painful or hard lymph nodes.
- Fever, fatigue, or night sweats accompany the swelling.
- Gum health continues to decline.
- Visible pus, abscess, or loose teeth.
Better safe than sorry. Treating gingivitis early often prevents the need for more aggressive interventions later.
FAQ Section
Can gingivitis cause swollen lymph nodes under the jaw?
Yes, gingivitis can cause swollen lymph nodes under the jaw if inflammation or infection spreads from the gums to the lymphatic system.
How long do lymph nodes stay swollen from gum disease?
If treated early, they may return to normal within a few days to a week. Chronic gingivitis or periodontitis may lead to longer-lasting swelling.
Are swollen lymph nodes always a sign of gingivitis?
No, lymph node swelling can result from various infections, autoimmune diseases, or even cancer. Gingivitis is just one possible cause.
Can natural remedies help reduce gum inflammation and lymph node swelling?
Yes, natural remedies containing neem, clove oil, and Omega fatty acids have shown promising results in reducing inflammation and promoting gum healing. You can try our gum disease oral solution for best results.
Is brushing enough to reverse gingivitis?
Brushing helps but may not be sufficient alone. A comprehensive routine including flossing, rinsing, and using targeted natural remedies is more effective.
Can gingivitis spread if left untreated?
Yes, untreated gingivitis can lead to periodontitis, tooth loss, and systemic infections that may affect your overall health.
Final Thoughts
So, can gingivitis cause swollen lymph nodes? Without a doubt. Your mouth is the gateway to your body, and what happens there can ripple out into your entire system. If your gums are bleeding, your breath is off, and you’re noticing swollen nodes near your jaw, it’s time to listen to your body.
While good dental hygiene is the cornerstone of gum health, integrating a natural, botanically-infused product such as The Goodbye Company gum disease oral solution into your routine can provide the extra support your gums need. Don't wait for things to escalate. Your lymph nodes are already doing their job - now it’s your turn.