You scratch your skin. You’ve dealt with the itch, the flaking, the flare-ups. But then one morning you notice your gums are bleeding, red where they used to be a healthy pink. Maybe they feel swollen. And you wonder, is this just poor brushing or something more, something tied to that psoriasis you have on your elbows, knees, scalp?
Can psoriasis affect your gums might sound like a weird question - like trying to connect dots between your skin and your mouth. But more and more evidence is saying: yes, psoriasis can reach further than you think. Underneath that barrier of skin lies inflammation, immune signals, systemic changes. And your gums are not immune (pun intended) from that ripple.
I want to walk you through what we do know, what’s still murky, what signs to watch for, and importantly, what you can do - natural methods, routines, and yes, a product that helps. Because if you’re already suffering from bleeding gums, tooth pain, or sensitivity to hot/cold, you don’t need just theory; you need relief.
What Is Psoriasis Beyond the Skin: The Ripple Effect
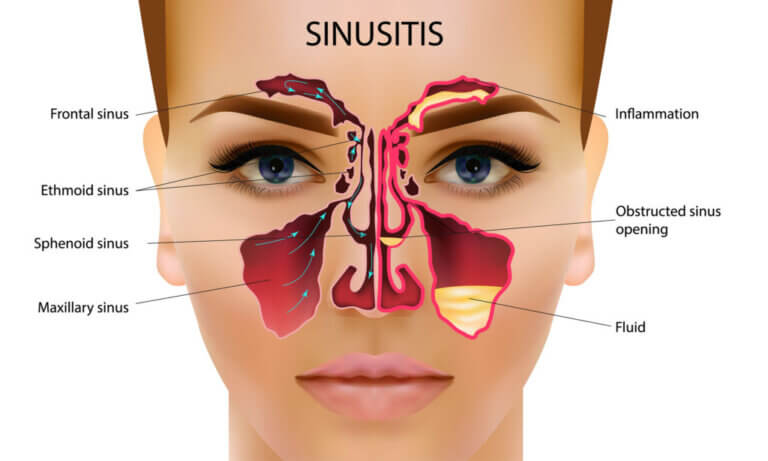
Before we zoom in on gums, let’s understand how psoriasis isn’t just a skin problem. It’s an autoimmune, inflammatory condition. That means your body’s immune system is misfiring, overproducing skin cells, creating plaques, but also circulating inflammatory markers throughout the body.
-
Psoriasis often comes with elevated levels of cytokines (like TNF-alpha, IL-17, IL-23) that don’t stick to just your skin. These can affect tissues elsewhere, including in your mouth.
- There’s also a higher prevalence of comorbid conditions: cardiovascular disease, arthritis, metabolic syndrome. That tells us the systemic inflammation is real.
Why might your mouth care?
Your mouth is full of bacteria. When everything’s balanced, they’re harmless, even helpful. But when your immune system is already on high alert (as in psoriasis), even mild bacterial shifts or small injuries (brushing too hard, food stuck in gums) can upset things more:
-
More gum inflammation.
-
More bleeding, because the blood vessels in gum tissue are sensitive.
- Possibly more bone loss around teeth if the inflammation is persistent.
Evidence That Psoriasis Is Linked to Gum Disease

What studies have found
Let’s look at what science has already uncovered — not always perfect, but enough to make you pay attention.
-
One study showed that people with psoriasis are about 4.4 times more likely to have gum disease than those without psoriasis.
-
Another found that in a group of psoriasis patients, 24% had moderate or severe periodontal disease, vs ~10% in a control group without psoriasis. Even after adjusting for smoking and dental care frequency.
- Bone loss: 36% of people with psoriasis had one or more areas of bone loss ≥3 mm compared to 13% in people without psoriasis.
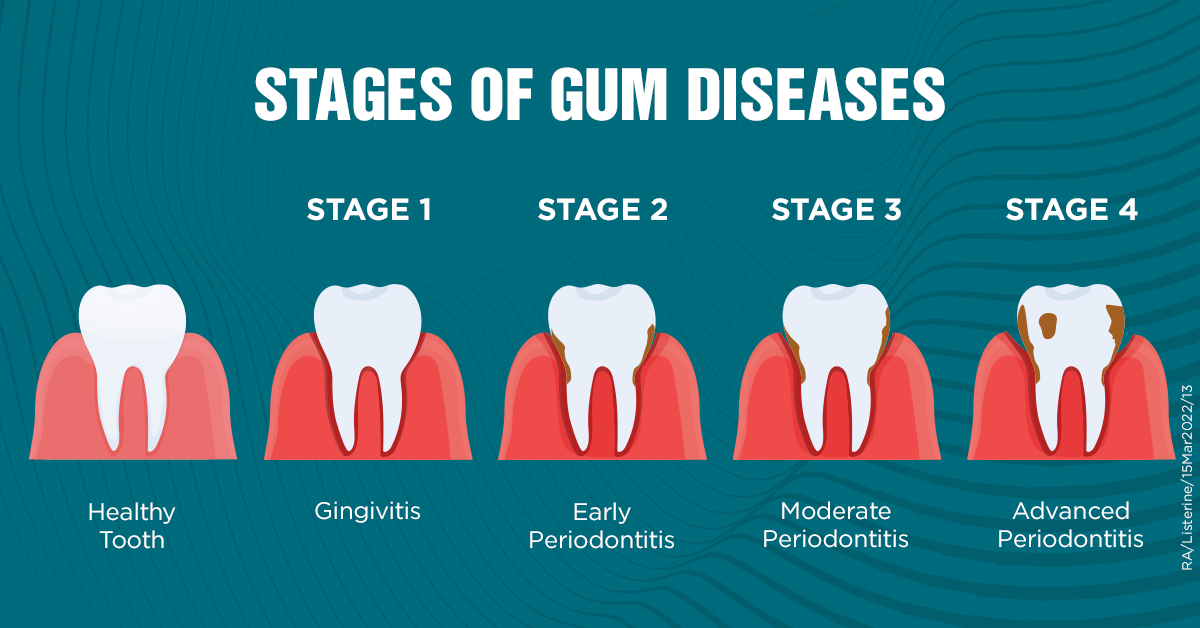
Symptoms And Early Warning Signs in the Mouth
You might not always notice something until it’s bothersome. But catching things early makes treatment easier, more effective.
Common Signs to Watch For
-
Bleeding when brushing or flossing - more than just once in a while.
-
Red, swollen gums, especially around the gum line.
-
Tender or sore gums.
-
Gum recession (gums pulling away from teeth).
-
Persistent bad breath not helped by regular brushing.
- Pain or sensitivity to hot or cold.
Less Common But Important
-
Lesions or patches inside the cheeks or on the tongue (in rare cases of oral psoriasis).
-
Peeling or fissured tongue, geographic tongue appearance.
- Difficulty eating spicy or acidic foods because your gums or mouth interior are too sensitive.
Shared Risk Factors And The Bi-Directional Link Between Psoriasis And Gum Disease
This is where things get interesting and a bit messy. Because it's not just that psoriasis can affect your gums; bad gum health might feed back into psoriasis. And there are a bunch of shared risk factors.
Risk Factors
-
Smoking: major risk amplifier. In studies, people with psoriasis who smoke have more severe gum disease.
-
Poor oral hygiene: irregular brushing, infrequent flossing, no dental cleanings.
-
Diet & nutrition: high sugar, processed foods may worsen both psoriasis flares and gum disease. Low intake of anti-inflammatory foods seems to correlate with worse oral health in psoriasis sufferers.
-
Obesity, metabolic syndrome, diabetes: conditions that add more inflammation.
- Genetics & immune response: predisposition to overactive immune response plays out in both skin and gums.
Bi-Directional Effects
This means:
-
The inflammation from periodontitis (gum disease) can increase systemic inflammation, possibly worsening psoriasis.
-
Flare-ups of psoriasis may increase susceptibility to oral infections or reduce healing capacity.
Shared Features Between Psoriasis and Gum Disease
|
Feature |
Psoriasis (Skin/Mucosal) |
Gum Disease (Periodontitis / Gingivitis) |
Why It Matters |
|
Chronic Inflammation |
Overactive immune system - cytokines, plaques, skin thickening. |
Bacterial plaque - immune response, gum tissue damage. |
More overall inflammatory load in the body. |
|
Bone/Tissue Loss |
Psoriatic arthritis involves bone/joint damage; possible bone erosion beneath skin lesions. |
Loss of alveolar bone supporting teeth in periodontitis. |
Combined bone loss worsens oral function and jaw health. |
|
Bleeding |
Skin lesions may bleed or ooze; mucosal involvement may cause bleeding in the mouth. |
Gums bleed easily when inflamed or damaged. |
Signals tissue fragility, need for intervention. |
|
Shared Triggers |
Stress, smoking, certain medications, infections. |
Same: smoking, poor hygiene, diet, systemic health. |
Reducing triggers helps both. |
|
Healing Delay |
Immune response dysregulated; possible poorer healing. |
Inflamed gums heal slower; deeper pockets, infection. |
Increases risk of chronic damage. |
Is Oral Psoriasis Rare?

So, is oral psoriasis truly rare? Technically, yes - at least based on official diagnoses. But here’s the twist: it might be far more common than the numbers suggest. Why? Because it’s often misdiagnosed or overlooked. If your gums are bleeding or inflamed, most dentists lean toward gum disease. If your tongue looks patchy, you may hear “irritation” or “vitamin deficiency.” Very few clinicians immediately say, “Oh, this could be oral psoriasis.”
What This Means for Your Gums
Now, this circles us back to the bigger question: can psoriasis affect your gums? The answer is a solid yes. Even if oral psoriasis is stamped “rare” in medical books, your gums and oral tissues are still influenced by the same overactive immune system driving your skin psoriasis. That means gum inflammation might show up as a direct symptom of oral psoriasis, or as an indirect effect of systemic inflammation making you more prone to gum disease.
Both your skin and your gums act as barriers. They’re on the front lines against bacteria, trauma, food, and more. If psoriasis can flare on your knees from a tiny scratch (thanks to the Koebner phenomenon), it’s not a leap to imagine it popping up where gums meet teeth - an area constantly battling irritation.
To make it more confusing, oral psoriasis doesn’t look the same for everyone. Some notice red, inflamed gums. Others feel burning or soreness, while a few develop geographic tongue (smooth red patches that look like a map). All these variations mean oral psoriasis can easily hide in plain sight.
So yes, oral psoriasis gets labeled as “rare.” But if you’ve got psoriasis and you’re noticing gum issues, you’re not imagining things. When you ask, “Can psoriasis affect your gums?” The reality is, absolutely - and possibly more often than statistics admit.
What Causes Oral Psoriasis in the Gums Vs External Psoriasis?
When you think about psoriasis, it usually shows up where everyone can see it - knees, elbows, scalp. But what about inside your mouth, specifically your gums? It feels odd, right? Yet, the same disease process that fuels those stubborn skin plaques can play out in your oral tissues. And that’s exactly why people ask, “Can psoriasis affect your gums?”
The Shared Immune Misfire
At the root of both skin and oral psoriasis is the same culprit: an overactive immune system. Instead of working like a disciplined army, your immune cells get a little reckless. They fire off too many inflammatory signals (cytokines like TNF-alpha, IL-17, and IL-23), which in skin leads to thick, scaly plaques.
In your gums, however, that same immune chaos looks different. The tissue there is thinner, constantly exposed to bacteria, food particles, and micro-injuries from brushing or chewing. So instead of building thick plaques like on elbows, the gums may respond with swelling, redness, bleeding, or painful patches.
Local Triggers Make the Difference
Another factor is local irritation. Your gums are constantly under fire - brushing, flossing, food rubbing against them, plaque buildup. If you already have an immune system on high alert thanks to psoriasis, those tiny irritations can flip the switch into a flare. That’s why someone might never see psoriasis inside their mouth, while another person develops what looks like angry, inflamed gums overnight.
There’s even something called the Koebner phenomenon - psoriasis lesions appear in places where the skin (or in this case, gum tissue) has been injured. For your knees, that could be a scratch. For your gums, it could be aggressive brushing or even dental work.
Why Oral Psoriasis Looks Different Than Skin Psoriasis
Skin plaques are easy to spot: thick, silvery, scaly patches. Oral psoriasis? Much trickier. In gums and mouth tissues, the environment is moist, delicate, and exposed to bacteria. That changes how psoriasis manifests. Instead of scales, you might see:
-
Smooth red patches that burn when eating spicy food.
-
Gum peeling or bleeding.
-
Geographic tongue (red map-like patterns).
-
General soreness or sensitivity.
So even though both conditions come from the same immune dysfunction, the way they play out depends on the environment - tough outer skin versus sensitive oral tissue.
So, Can Psoriasis Affect Your Gums in a Unique Way?
Absolutely. When psoriasis shows up in your gums, it’s like the same storm hitting a different landscape. The underlying immune overactivity is the same, but local triggers and tissue type change the outcome. That’s why oral psoriasis is often harder to recognize and diagnose, and why gum problems in psoriasis patients deserve more attention than they usually get.
If you’ve got psoriasis and your gums feel off - bleeding, painful, or unusually inflamed, don’t brush it off as “just brushing too hard.” It could be another way psoriasis is making itself known. And once again, the big question “Can psoriasis affect your gums?” gets a pretty clear answer: yes, in more ways than one.
Can Psoriasis Treatment Help Oral Symptoms?
If you’re already treating psoriasis on your skin, you might wonder: does that same treatment calm things down in the mouth too? The short answer - often, yes. But it’s not always straightforward, because gums and oral tissues respond a little differently.
Systemic Treatments: One Stone, Two Birds
The good news is that systemic treatments (the ones that work throughout your whole body) don’t discriminate between your elbows and your gums. Medications like biologics (think adalimumab, secukinumab, ustekinumab) and traditional drugs like methotrexate or cyclosporine target the overactive immune response everywhere.
So if you’re taking one of these, you may notice that both your skin plaques and your gum irritation improve. Many patients report fewer gum flares once their systemic treatment is under control. In other words, if you’ve been wondering, “Can psoriasis affect your gums, and if so, will my biologic help?” The answer is usually yes, it can help tame both.
Topical vs Oral Tissue Challenges
Here’s where it gets tricky: topical treatments like steroid creams or ointments are staples for external psoriasis. But gums aren’t exactly the best place to smear on medication. The mouth is moist, saliva washes things away, and gums are delicate. That makes traditional topicals less effective or harder to use.
Dentists or dermatologists sometimes prescribe steroid rinses, gels, or sprays that are designed for oral tissues. These can help calm inflammation directly where it hurts, but they often need to be used carefully to avoid side effects like fungal infections (thrush).
Dental Care as “Treatment Support”
Another overlooked piece? Dental hygiene and routine care. While not a “psoriasis treatment” per se, professional cleanings, gentle brushing, and good flossing can reduce gum irritation. Since gum tissue is already vulnerable when you have psoriasis, minimizing plaque and bacteria makes it easier for medical treatments to work.
Think of it as teamwork: systemic meds calm the immune storm, and good oral care removes the local triggers that would otherwise keep adding fuel to the fire.
Why Results Can Vary
Not everyone sees the same improvements in their gums, even on powerful biologics. Some patients get clear skin but still notice oral flare-ups. Why? Because local irritants - like dental trauma, infections, or even spicy foods, can continue to provoke gum issues regardless of how well your psoriasis is controlled systemically.
So while treatment often helps, it’s not a one-size-fits-all solution. If you feel your gums aren’t catching up while the rest of your psoriasis is improving, it’s worth flagging this to both your dermatologist and dentist.
Can Treatment Help?
If your gums are hurting and you’re thinking, “Can psoriasis affect your gums, and will treatment fix it?” The answer is yes, treatment can make a noticeable difference, especially when combined with consistent dental care.
Are the Gums Directly Infected in Psoriasis?
No: psoriasis itself is not an infection caused by bacteria or viruses. But infection (bacterial plaque) in the gums can worsen when the immune system is dysregulated. So the disease in gums is often periodontitis / gingivitis rather than psoriasis directly affecting that tissue — though in rare cases oral psoriasis lesions can appear on gums or nearby mucosa.
Why Some Gums Fare Worse: Specific Challenges in Psoriasis
Let’s dig into what makes gum issues worse for people with psoriasis, beyond the shared risk factors. Because not everyone with psoriasis has awful gums - but certain things increase the odds.
Immune Dysregulation & Healing
-
The mis-timed immune response means that even small gingival irritation (food stuck, plaque) might provoke a stronger response, more swelling.
- Healing from gum disease treatments (deep cleaning, scaling, etc.) may be slower or less effective if your systemic inflammation is high.
Effects of Medication
-
Many psoriasis treatments include immune suppressants, steroids, or biologics. These can alter your body’s ability to handle bacterial loads or heal wounds. Sometimes dry mouth side-effects can reduce saliva, which normally helps cleanse and buffer the mouth.
- Some topical treatments (if used around the mouth) may irritate the rims or corners, increasing risk of secondary oral irritation.
Lifestyle & Psychological Stress
-
Psoriasis is visible, sometimes stigmatizing. People may eat differently (avoid social meals), may become depressed, maybe neglect oral hygiene during flare-ups.
- Stress itself is a trigger for psoriasis, and stress causes changes in immune signaling and saliva production, which then worsen gum health.
Protecting Your Gums When You Have Psoriasis: What to Do?
Alright - enough about problems. Let’s talk about solutions. What you can do, right now, to reduce the risk, soothe existing issues, and improve both skin and gum health.
Build a Good Oral Hygiene Routine
-
Brush twice a day, with gentle but thorough technique. Soft-bristled brush.
-
Floss daily - don’t skip those interdental spaces.
-
Use an antiseptic mouthwash (check with your dentist) to manage bacterial biofilm.
- Regular dental cleanings (every 6 months or more often if your dentist advises).
Dietary & Lifestyle Adjustments
-
Eat anti-inflammatory foods: oily fish (rich in Omega-3), leafy greens, fruits (especially berries), nuts.
-
Reduce sugar and refined carbs — because plaque thrives on sugar.
-
Quit or reduce smoking. Also limit alcohol.
- Stay hydrated, reduce stress. Use techniques like sleep, relaxation, maybe meditation.
Be Proactive with Your Health Team
- Let both your dermatologist and dentist know that you have psoriasis - full body/system involvement.
- Ask them whether your current psoriasis treatments might impact your oral health (meds, side effects).
- If you see new symptoms in your mouth/gums, don’t assume it’s just “nothing”, get it checked.
Introducing The Goodbye Company Gum Disease - A Natural Helping Hand
If you currently suffer from poor oral health, such as bleeding gums, tooth pain, sensitivity to hot or cold - you deserve something beyond gentle advice. Something that helps.
That’s where The Goodbye Company Gum Disease oral solution comes in. It’s not just another toothpaste or rinse. It’s an all-natural preventative oral care solution designed to prevent and treat gingivitis, infused with Omega-3 and Omega-9 oils, along with neem and clove essential oils. These ingredients are chosen because:
-
Omega-3 & 9 are known for anti-inflammatory benefits; reducing tissue inflammation and supporting healing.
-
Neem has antiseptic properties; helps reduce smell, kill harmful bacteria.
- Clove oil provides pain relief, antibacterial effects, and helps numb sensitivity.
If your gums are already troubled - bleeding, swollen, sensitive, using a natural gum health-supportive product like The Goodbye Company Gum Disease daily can complement your brushing/flossing/cleaning. It’s part of a holistic oral care routine.
Use it morning and night after brushing, and consider a gentle massage of your gums. You might find that combining it with better diet, oral hygiene, and managing psoriasis flares gives you noticeable relief.
FAQs - Can Psoriasis Cause Gum Disease?
Can psoriasis cause gum disease - Directly?
Psoriasis does not directly “cause” gum disease in every case, but it increases your risk. The systemic inflammation, immune dysregulation, and shared risk factors (like smoking, diet, hygiene) make gum disease more likely in people with psoriasis.
What are the symptoms of oral psoriasis?
Symptoms can include red patches, burning or soreness, bleeding, gum peeling, sometimes lesions in the mouth. If you already have skin psoriasis, seeing changes in your mouth or gums (redness, swelling, irritation) should prompt a check with your dentist or dermatologist.
Can treating gum disease improve psoriasis?
There is some evidence suggesting that reducing oral inflammation may help with overall inflammation in the body, possibly lessening the severity or frequency of skin psoriasis flare-ups. The direction of causality isn’t crystal clear yet.
Outlook
So, can psoriasis affect your gums? The answer: yes, absolutely. It isn’t guaranteed in every case, and there are many variables (severity of psoriasis, lifestyle, hygiene, genetics), but the link is strong enough that you should treat it as real, not theoretical.
Make sure that you keep tabs on your mouth. Use natural aids like The Goodbye Company Gum Disease oral solution to help soothe, heal, and prevent, and collaborate with your healthcare team to reduce inflammation.