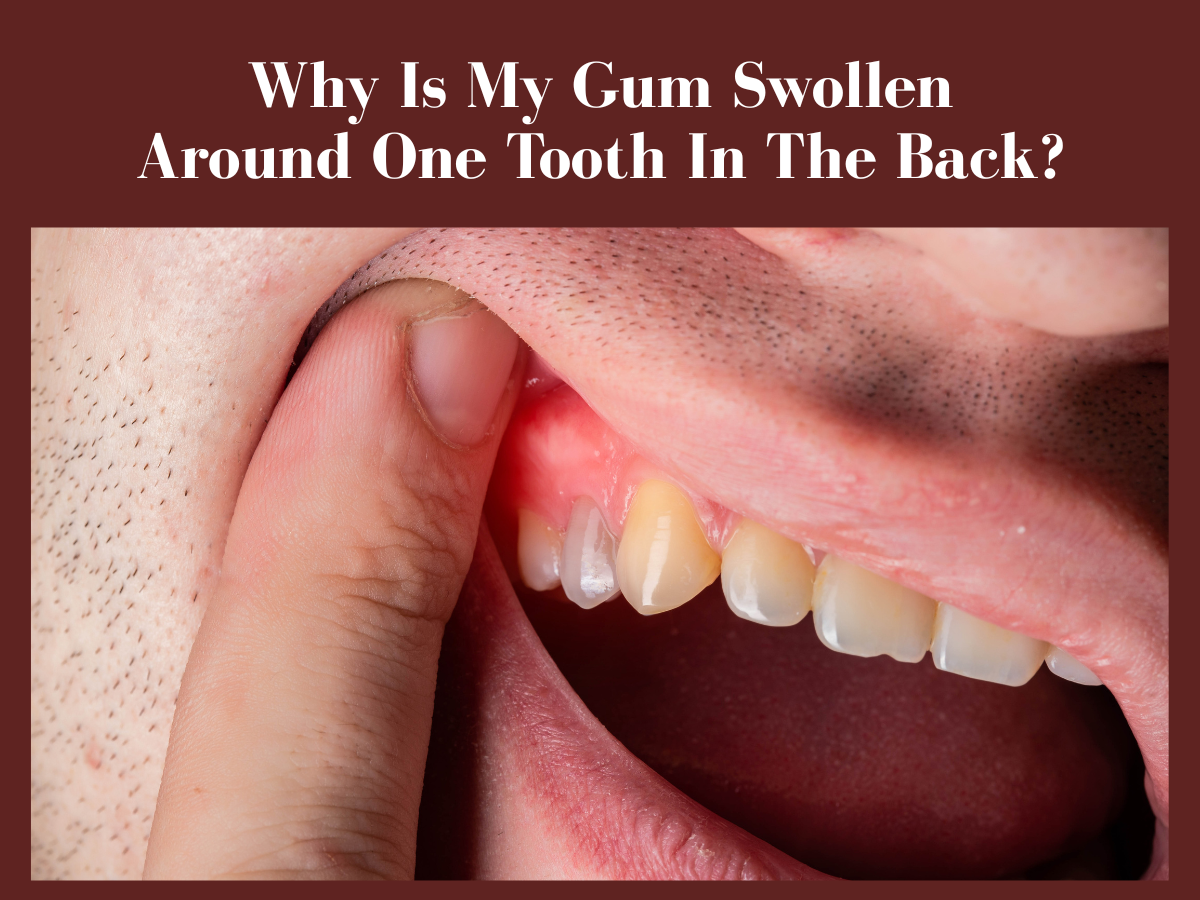
You may be grinding for your career or living the life of your dreams until one morning, your toothbrush hits a sore gum. Ouch-that pain is enough to jolt you awake. But are you thinking of turning a blind eye to it because of your busy schedule and assuming it will heal on its own? Do you think a swish of your mouthwash or another swipe of a toothbrush will settle the puffiness? Well, the matter is far beyond oral hygiene. Swollen gums are nothing you should brush off because it's your body's way of signaling 'something's not right under the root.
They say: Where there's smoke, there's fire—so is the gum swelling. Periodontal inflammation is not only a matter of apparent symptoms like redness, puffiness, and throbbing pain, but a lot more is happening around and under the tooth. Maybe there's some plaque accumulation, an infection, or a root fracture that's causing gingival irritation. All you need is a thorough investigation of the culprit and timely intervention before bleeding, bad breath, and tooth decay become uninvited guests.
Explore below the SOS signals your mouth is flashing and the possible reasons behind this hitch. Also, look out for the dentist-approved quick fixes in the end—because trust me, you don't deserve to be in pain.
Your Gum's SOS Signals:
Inflammation is actually your ally in disguise. It is a cascade of defense responses against a particular stimulus (the culprit), wherein the scene your body sends an army of immune responders and inflammatory mediators to begin the turmoil—the war that seeks to create peace in your mouth. But instead—arises certain concerns that prevail until you solve the root cause.
Not only the pain, but your gums also alter the way they look. Your gingiva now becomes red to purplish instead of being beautiful, healthy pink. You may also notice a change in the landscape of your gums that transforms from firm and fit to tender and soft—it's another indication that your gumline is in danger. As the swelling snowballs, your tooth bed may become so tender that it may bleed easily— most often, when you brush hard or accidentally hit the victim tooth in the back.
If you don't pay attention, assuming it's only one tooth- no big deal - you may lose your tooth. I mean, ignoring this periodontal issue is like letting the mouth termites feast on your dental fortress. Luckily, this dental degradation occurs gradually, but if it remains untreated, the inflammation aggravates and leads to several periodontal issues, eventually causing gum recession and exposing dental roots. Those uncapped roots then become seriously sensitive, throbbing, and stinging when you eat or drink something really hot or frosty cold.
The chaos does not end here-the sore tooth begins to lose support from its root structure and may eventually fall away anytime, just like a dead leaf drifting from its branch. Though it's the end of the showdown, it has certain consequences that appear in the long run if you still do not heed. The toll comes from the lack of support for adjacent teeth, which gradually misaligns and deforms the dental framework.
So, the lesson of the story is you must guard the gates before the enemy marches in because a few minutes of dental care can save you years of repair.
Why is it always the 'Pinky Tooth'?
So, your gum has raised the SOS signals, but have you ever wondered why the alarm almost always rings at the very back? Why is it always the pinky tooth, just like the pinky finger, that always gets hit and complains I didn't see that coming? I think the answer is quite apparent, and most of you already knew that it's actually really hard to reach the corners, particularly when you are using the wrong size of your toothbrush-I mean, the bigger one than what your jaw can slide into the sides.
Perhaps you are not using the right tools/products or the proper techniques for oral hygiene, and somehow your food particles remain stuck in between your teeth at the back. Gum swelling may also happen when you enthusiastically try to scrub every nook and cranny of your jaw and accidentally hit your gum really hard. Ouch! That stinging pain shoots through your gums, making you freeze mid-brush—my condolences for your pinky tooth.
Sometimes, the problem is not that the farthest molars do not get cleaned the way they should be. The toll comes from your impacted wisdom tooth that does not bring wisdom but nuisance. It is when your last molars try to make their grand entrance in a breech position—the struggle can irritate the surrounding gingival tissue, leading to redness, puffiness, and a dull-aching pain.
What Ignited Gum Swelling? The Real Culprits Behind The Curtains
So, you know that your gumline doesn't flare up out of the blue; there's always a concern that needs to be addressed. To understand yours, look up the following common to rare problems and check off anything that applies to you, because when you know the why, you can handle the what.
Plaque & Tartar Infiltration
Plaque buildup is a natural phenomenon, and it's inevitable. Sounds strange? Yeah, it is. Every day after you brush, your saliva creates a protein-based film—the pellicle on your teeth. This thin film is designed to protect your tooth enamel from acids and toxins that may come from food or the microbiome of your mouth. Unfortunately, this pellicle proves to be a blessing in disguise, becoming a landing pad for the bacteria. The filthy microbe easily anchors, occupies, invades, and multiplies as if it were its own territory.
The abundant colonies of newly-born bacteria, the residual food particles, and the saliva- all create a sticky biofilm which you call plaque. If you do not remove this microbial mat, the invisible invaders in it will multiply progressively, feeding on the sugars from your food and releasing acids and toxins that not only damage your tooth enamel but also irritate your gums. The more germs, the more damage.
Moreover, if you don't brush or floss your plaque away, it will fossilize into tartar, layer by layer. This happens when minerals like calcium and phosphate from your saliva slowly deposit on the biofilm. These mineral ions gradually crystallize and form a hard, pale-yellow to grayish green, cement-like structure, which you call calculus or tartar.
So this is how you let your biofilm build its unbrushable fortress. Remember, by this stage, you can't remove the hardened plaque (calculus) through brushing or flossing—you will need professional scaling, the dental procedure that breaks the calcified wall to rubble.
Food Lodgment & Local Irritation
If you recall from earlier, plaque contains an army of bacteria that feeds on fermentable carbs from your meals. So, when you don't brush and floss religiously, the tiny food particles wedged between your teeth become the spoils of war on which these microbes thrive and flourish—causing you all kinds of trouble, from puffy gums to cavities and even tooth loss.
Sometimes, the problem isn't just the crumbs stuck between your teeth fueling bacteria—it's also the irritants from ultra-processed foods that provoke and sensitize your oral mucosa. These irritants include acids, additives, preservatives, and flavoring agents that may alter the pH and damage the epithelial cells of your gumline, causing them to puff up and rise in rebellion.
Mechanical trauma and Impacted Wisdom Tooth
Brushing too firmly or snapping the floss too aggressively can harm your soft gingival tissue, making it sore and even bleed, particularly if the hit is terribly hard. Such inflammation usually settles on its own within a few hours or days, so there's no need to worry if that's what you are experiencing. Give your gums a little time—and trust them to win the battle on their own.
However, sometimes a careless jab from a sharp tool—say, a toothpick—can scrape your delicate gum lining and leave behind a blister that does not go away until you scream in pain for days and weeks. These mouth ulcers don't just sting you with pain; they turn every word and every bite into a challenge, until you finally call on topical anesthetics or mild steroid ointments to take control.
At odd times, when you least expect it, the trauma creeps in from your so-called wisdom tooth, especially the impacted one that seems to have no wisdom at all. It doesn't care if your jaw has room; it slyly shoves its neighboring molars, determined to erupt at any cost. This kind of impaction exerts a deep pressure on your soft gingiva, causing it to swell and create a pocket for infection.
The 'well' is actually the flap of swollen gum above the impacted wisdom tooth— a perfect pocket that traps food particles and feeds the lurking bacteria within. As the microbial army multiplies, your immune cells grow furious and fight back to wipe them out. The battle leaves behind countless fallen bodies of the germs and guards, forming a foul-smelling pus within the well. The abscess, in turn, aggravates gum inflammation, requiring a dentist to step in and treat the infection.
Medical & Medication
Many a time, the trouble is not the poor oral hygiene or improper dental care, but there may be some other real culprit lurking deep within your body. In fact, there's a maze of medical conditions that can transform the terrain of your mouth, making your gums puffier, tender, and hypersensitive.
If you are a girl, you know exactly what that pain feels like— the time when you are already weathering the storms of menstruation or pregnancy, and then you have to face the trial of swollen gums. The culprit isn't menstruation or pregnancy itself; these are simply part of the beautiful journey of womanhood. It's actually the rush of hormones that increases blood flow towards the soft tissues of your oral mucosa, making them more sensitive and causing them to puff up in response.
Moreover, if you are navigating life with diabetes, sadly, your dental health becomes a real challenge. Elevated blood glucose levels, compromised immune system, reduced blood circulation, and often dry mouth (xerostomia) —all these factors contribute to supporting the proliferation of bacteria in your mouth, leading to several dental issues, such as gingivitis, periodontitis, and periodontal disease. Meanwhile, similar sequelae appear if you are dealing with any of the autoimmune diseases or blood disorders.
An often-overlooked yet silent offender is scurvy, which is a disease born from severe vitamin C deficiency and lack of collagen production. Without enough vitamin C, your gums lose strength and integrity, becoming more fragile and susceptible to bleeding. This is what you call vitamin deficiency gum swelling.
And then there's the medication side of the story, where the side effects or adverse effects of the medicine cause drug-induced gingival hyperplasia or gingivitis. Certain drugs, such as calcium-channel blockers (the drugs used to control blood pressure), anticonvulsants (like phenytoin), and immunosuppressants such as cyclosporine, trigger Drug-Induced Gingival Overgrowth (DIGO). Even the medicines used to control birth (oral contraceptives) and the drugs used to manage depression (antidepressants) can tweak your hormonal levels, causing gum swelling and bleeding.
Periodontal Disease
Periodontal disease is one of the most common causes of localized gum swelling. It's a progressive infection that weakens the integrity of your mouth's natural guards—the bones, ligaments, and gums that support your teeth and frame your jaw. Initially, the infection is mild and remains confined to the gumline, where the bacteria in the plaque irritate the gingival tissue, making it swollen, tender, firm, and painful.
But if you fail to heed the alarm or slay the villain while it's weak, you may end up advancing the bacterial invasion deep within the roots. The unchecked bacterial siege then breaches the gingiva and invades the bones and supporting ligaments, creating pockets of pus along the way, eventually leading to what's known as periodontitis— the advanced stage of gum inflammation.
Dental Abscess & Infection
Gum inflammation around one tooth can sometimes appear because of a dental abscess— a tricky term, indeed—so let's simplify it. A dental abscess is a clinical name for a localized pocket of pus that forms when bacteria in your mouth proliferate and invade the soft tissues around a tooth or the gum.
Most precisely, when the infection spreads to the tooth pulp, it's called a periapical abscess, whereas when the pus accumulates within the gumline, it's known as a periodontal abscess. In the case of a periodontal abscess, dead cells of the bacteria and immune responders accumulate to form painful, hard lumps within your gums, throbbing you with deep pressure and discomfort. It's not just the pain; this kind of infection also brings along foul breath and an unpleasant taste. Though localized at first, such infections can spread to nearby teeth if left untreated.
Dental Restoration & Post-procedures
Sometimes when your mouth goes through dental work, your gums may protest in response. It's often because they've been forcefully nudged or nicked during the procedure, which makes them look puffier and more tender. Well, this kind of swelling, irritation, and redness usually fades within a few days.
However, it's also possible that your gums are reacting to a material used by your dentist—maybe the resin, filler, or a bonding agent—and they begin to swell and sore. Or perhaps it's an overhanging restoration, where the new filling or the crown just extends a little too far over your tooth's edge–creating a campsite for bacteria to thrive happily on trapped food particles until your immune guards begin to counterattack and your gums swell in rebellion.
Well, don't panic—this kind of localized gum swelling is just a temporary protest, and it usually settles within a few days. However, if it lasts for longer— remember it's your gums' SOS signal—time to call your dentist to smooth out his work.
DIY Dental Peace: Home Remedies To Heal Naturally
Before you call your dentist to take charge, try a few easy-peasy DIY home fixes first. Many of these soothing solutions are probably available in your kitchen— 100% natural, organic, and proof that nature has its own way of healing. However, when nature's touch isn't quite enough, modern medicine can step in to help—so you might want to try a few chemical cures that, when used correctly, can be real game-changers.
Salt Water Gargle
A warm salt gargle is just like a mini spa for your gums—warm, soothing, and cleansing. It's that one remedy the whole world seems to agree on, the universal go-to cure people reach for first, no matter what the oral problem they face. You can join the crew too—simply rinse your mouth with this magical solution. Just add half a teaspoon of salt, which is a natural antiseptic, to about 150 mL of warm water, and gargle it around for 30 seconds to soothe your gum inflammation and soreness. Repeat the rinse two to three times a day for the best results.
Ice Packs/Cold Compresses
A slightly less effective yet still reliable option for mild gum swelling around one tooth is a cold compress or an ice pack—whichever you prefer. Both work, but differ in convenience. As an ice pack is a ready-made solution; just take it out of the wrapper, apply it to your outer cheek, and feel the relief from the pain.
On the other hand, you may need to prepare your own cold compress, for which you'll need a clean soft cloth and a few ice cubes. Simply wrap the ice cubes in the cloth and gently dab them on your cheek for two to three minutes. Repeat according to your tolerance to cold and wait till the magic happens. Trust me, if you have a mild sore gum around a back molar or a wisdom tooth that isn't impacted, this simple and quick remedy might be all you need.
Oil Pulling
If you believe in and practice Ayurveda, oil pulling is an excellent, practical solution for you. Oil pulling uses edible oils, such as coconut oil, sesame oil, or sunflower oil, with the conviction that swishing it in the mouth for several minutes—let's say 15-20 minutes—helps remove bacteria, plaque, and food debris from every nook and cranny of your jaw. Although this practice lacks strong scientific evidence, which is why dentists don't recommend it, it's becoming a trend on social media, often without mentioning its side effects and related risks. For instance, spitting the oil after rinsing your mouth is essential, or else it will upset your GI tract.
Moreover, this practice may cause gum swelling and increase the sensitivity of your teeth, despite actually soothing the inflammation. What I have learned so far about this natural cure is the principle of 'like dissolves like'— meaning the oil has the capacity to dissolve the phospholipid membranes of bacterial cells, a key interaction that helps detach the biofilm from your tooth surface. So, while this remedy may not completely soothe your gum inflammation, it may still contribute to removing plaque from between your teeth that may be causing your gums to swell.
Clove Oil
You might have seen advertisements or labels on your toothpaste tubes claiming to have clove bits or clove oil in them—that's because of the many great benefits of clove oil. This natural elixir actually contains eugenol, which is a powerful antiseptic, analgesic, and anti-inflammatory. It's quite safe and easy to use, and has no side effects unless you ingest it for some other purpose without diluting it to the prescribed ratio.
For oral application, however, you don't necessarily need to dilute it— just grab a small, clean cotton ball, soak it in some clove oil (don't forget to wring it out to avoid ingestion), and place it directly on your swollen gum. Leave the oil-soaked ball on the affected site for about 5-10 minutes, and let nature do its job.
Turmeric Paste
Turmeric isn't just a spice— this nature-powered blend works wonders when it comes to healing, particularly when it's a matter of inflammation, because turmeric contains curcumin, a potent anti-inflammatory and antioxidant. So when you apply this soothing golden paste to your swollen gums, the puffiness and redness fade away like they never happened.
To make this golden blend, mix half a teaspoon of freshly ground organic turmeric with a few drops of mustard oil—just enough to make a thick paste. Clean your finger, or use a cotton swab, to apply this mixture to your inflamed gum and leave it for about 5-10 minutes. Then clean your mouth with lukewarm water, and repeat this ritual twice daily until your gingiva heals.
Aloe Vera Gel
You may not be unaware of the cooling and calming effects of aloe vera gel. It's nature's band-aid that comes straight from the pulpy leaves of the succulent plant called Aloe barbadensis. The cooling green balm is an excellent therapy for swollen gums near wisdom teeth due to its powerful anti-inflammatory, antibacterial, and soothing properties.
It's as simple to use as it sounds—just scoop out some fresh aloe gel from your plant, or, if you don't have a natural one, opt for a fragrance-free and alcohol-free aloe gel from the market. Using your clean finger, apply the gel to your irritated gingival tissue and leave it for about 5-10 minutes. Then gargle your mouth with lukewarm water, and repeat as often as you wish—it's a calming, soothing salve with no harm done.
Hydrogen Peroxide Rinse
Fizz away the bacteria in your mouth with some bubbles of hydrogen peroxide- a remedy that sits right between science and simplicity. Hydrogen peroxide is a gentle antiseptic that helps remove plaque from your teeth, which means it may not directly soothe your gum inflammation, but it does tackle the root cause, as gum swelling often occurs due to plaque buildup or bacteria lurking in the cavities of your tooth.
For this quick swish, mix equal parts water and 3% hydrogen peroxide. Gargle this sparkling liquid for about 30 seconds, then spit it out—never swallow this chemical. You can repeat this rinse once daily for a few days and monitor if it helps calm your inflamed gingiva—otherwise, look for the deeper cause that may urgently need correction.
Antiseptic Mouthwash
If you think oral hygiene is the issue, don't wait— start practicing proper dental care before it's too late. Brush your teeth twice daily—once in the morning and once before bed. However, if you eat something sweet, make sure you brush afterward. Floss daily and use a good-quality mouthwash for a more powerful cleansing effect.
Over-The-Counter Medication
Planning a dental visit but hoping to ease your gum pain and soreness in the meantime? Try over-the-counter medications such as ibuprofen or acetaminophen—quick and effective pain relievers that are easy to use on the go. These medications provide temporary relief from inflammation and pain—so it's important to address the underlying cause; otherwise, the soreness will return once the medications' effects wear off.
Time To Call In Reinforcements
When to See Your Dentist
If no home remedy or OTC medication brings relief and your gums continue to swell, ache, and bleed for more than a few days, it's time to call in your dental cavalry. Because there are things only a professional can do better— for instance, scraping away stubborn tartar, which is impossible to remove at home.
Sometimes, there may be a gum abscess that needs to be drained professionally to prevent the infection from spreading. In other cases, your gum inflammation may stem from an advanced stage of periodontitis—a condition that requires a skilled professional to plan procedures like scaling or root planing. And at times, it may be an impacted wisdom tooth causing gingival soreness—and the only real cure is tooth extraction that relies entirely on your dental surgeon's expertise.
The Diet That Builds Dental Defense
Here's your gum-care cheat sheet—take a peek into what your gums love and what foods make them sore.
|
FOODS YOUR GUMS LOVE |
|
|
Food Options |
Advantages |
|
Crunchy fruits and vegetables |
Rich in antioxidants and vitamins-promotes overall oral health, act as natural toothbrush |
|
Leafy greens |
Contains calcium, antioxidants, and are rich in vitamin C-promotes collagen production and strengthen gingival tissue |
|
Dairy products |
Contains calcium and casein- strong teeth and healthy gums |
|
Berries and citrus fruits |
Rich in vitamin C and antioxidants- boosts immune system, increases blood flow, and accelerates repair of wear and tear |
|
Nuts and seeds |
Rich in omega fatty acids, vitamin E and D- the goodness that fortifies gum health |
|
Garlic and onions |
Not everyone's favorite due to their pungent flavor and aroma, but are natural antiseptics that help fight off bacteria |
|
Fatty fish |
Rich in omega-3 fatty acids-supports immune system |
|
FOODS YOUR GUMS HATE |
|
|
Food Options |
Disadvantages |
|
Sugar (visible or hidden in the food, e.g., snacks, juices, soft drinks, and processed foods) |
Feeds oral bacteria, leading to plaque buildup and a chain of dental problems |
|
Starchy foods |
Starch breaks down to sugar (this part of digestion begins in the mouth)-breeding ground for oral microbiome |
|
Ultra-processed or junk food |
Contains hidden sugar, sodium, and trans fats-damage gums, teeth, and weaken immune system |
|
Acidic or spicy foods |
Acids erode tooth enamel while spicy foods irritates the gingiva |
|
Alcohol |
Dries out mouth, causes irritation, and gum swelling |
|
Tobacco |
Not a food— but a habit, in the form of betel quid or through smoking— weakens immune system and restricts blood flow |
Guarding The Gate: Habits That Protect Your Gums
Good habits grow healthy gums— but only when you truly take care of your teeth and gums. However, if you do not follow proper dental care, your oral health may decline gradually until you risk losing your teeth long before you reach 80. Here are a few basic hygiene practices you must follow to protect your gums.
-
Waxed flossing
Clear out plaque between your teeth and around the gumline regularly using a dentist-approved, waxed floss—waxed because it glides easily between teeth, especially if they are tightly placed or if you have braces.
-
Regular brushing
Brush twice daily—and especially after eating desserts. Use a high-quality toothbrush with soft, medium, or hard bristles, depending on how much plaque has accumulated on your tooth surface. Moreover, always brush at a 45-degree angle from your gumline, beginning at the back molars and working your way to the front teeth.
Move your brush in gentle, back-and-forth motions and try to cover every tooth. Also, don't forget to scrape your tongue clean after brushing—it's where most bacteria love to hide. You can also use an antiseptic mouthwash afterward, though many dentists advise caution, as some formulas may remove the fluoride coating from your teeth.
-
Oil pulling
You may practice oil pulling for extra oral care; however, never replace brushing and flossing with it. Think of it as a supplement, not a substitute.
-
Quit smoking
You should avoid smoking, as tobacco can weaken your immune system and suppress its ability to fight off bacteria and other infections. This weakness can ultimately lead to plaque buildup and a chain of dental problems— just as discussed earlier in the section "Your gums' SOS signals."
The Curious Corner
Can sore gums cause headaches?
Yes, sore gums can cause headaches— because the nerves in your jaw are directly wired into the brain. When these nerves become irritated due to a bacterial infection, the pain can radiate upward, triggering a headache. It may also be due to increased pain sensitivity resulting from an advanced stage of periodontal disease, which can make headaches more persistent.
How to treat gingivitis in pregnancy?
Pregnancy gingivitis occurs due to drastic hormonal changes, and there's not much you can do to stop them—except go the extra mile with your oral hygiene. Consider using a dentist-approved electric toothbrush to reach every corner of your mouth, and floss regularly with a soft, waxed floss to keep the gumline clean.
You can also visit your dentist more frequently during pregnancy, where your dental professional may prescribe you a pregnancy-safe mouthwash to deeply cleanse your mouth and eliminate bacteria that may harm your gums and teeth. Moreover, try to cut back on foods that promote bacterial growth and plaque buildup—such as sugary foods, starch, acidic foods, soft drinks, and spicy meals.
Swollen gum around one tooth in the back: Is it gingivitis?
Swollen gums may indicate gingivitis, but not always. The soreness or redness of your gingiva can be as mild as food impaction, plaque buildup, or irritation from acidic food. However, sometimes it's an early warning sign of a more serious problem, such as a gum abscess or periodontal disease.
So, if you notice your gum is swollen around one tooth at the back, begin with home remedies and pay close attention to your oral hygiene. If the swelling doesn't subside within a few days, visit your dentist to identify the exact cause—and follow the proper treatment accordingly.
Why is my gum swollen around one tooth, but no pain?
Pain in swollen gums usually occurs due to an infection or abscess. In cases of mild irritation, your gums may simply swell in protest— and all you need is something to calm or soothe your inflamed gums. So, no worries— just maintain good oral hygiene practice and give your gingiva a little time to heal. In the meantime, you can try using aloe vera gel, ice packs, or salt water rinses to ease the distress.
Gum swollen around one tooth overnight: Is it serious?
Usually, such a sudden response from your gums is an allergic reaction to spicy or acidic food, and you don't need to worry at all. However, sometimes, if the swelling progresses and makes you feel breathless, seek immediate medical attention, as it may be a severe anaphylactic reaction.
On the other hand, gum swelling around one tooth overnight may indicate that your gums are accumulating pus from an abscess, which needs to be professionally drained as soon as possible.
What is pericoronal flap swelling?
A pericoronal flap is simply an extra fold of gum tissue that partially covers a newly erupted or partially erupted wisdom tooth. This flap creates a small pocket between the gum and your tooth— a perfect spot for bacteria to hide and food particles to get trapped. Inside this space, mouth bacteria multiply rapidly, prompting your immune cells to respond and fight back. As the battle continues, the pus forms—a sign of infection known as pericoronitis that you should never ignore—because if left untreated, the infection may spread to your jawbone.